Emergency Medicine
Session: Emergency Medicine 9: Respiratory
232 - The association of the MeMed BV test with radiographic pneumonia in children
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 232
Publication Number: 232.3269
Publication Number: 232.3269
- SR
Sriram Ramgopal, MD (he/him/his)
Assistant Professor
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: The diagnosis of pneumonia using clinical examination and radiographic findings may be further enhanced via the incorporation of novel assays that more accurately differentiate between viral and bacterial pathogens. Studies have found conflicting results when examining whether biomarkers, such as C-reactive protein (CRP) and procalcitonin, can assist in the diagnosis of pneumonia. The recently-described MeMed BV test incorporates three biomarkers: C-reactive protein, interferon gamma-induced protein, and tumor necrosis factor-related apoptosis-inducing ligand, into a single assay to provide a risk estimate of bacterial infections.
Objective: To evaluate the association of the MeMed BV assay with the presence of radiographic pneumonia in children.
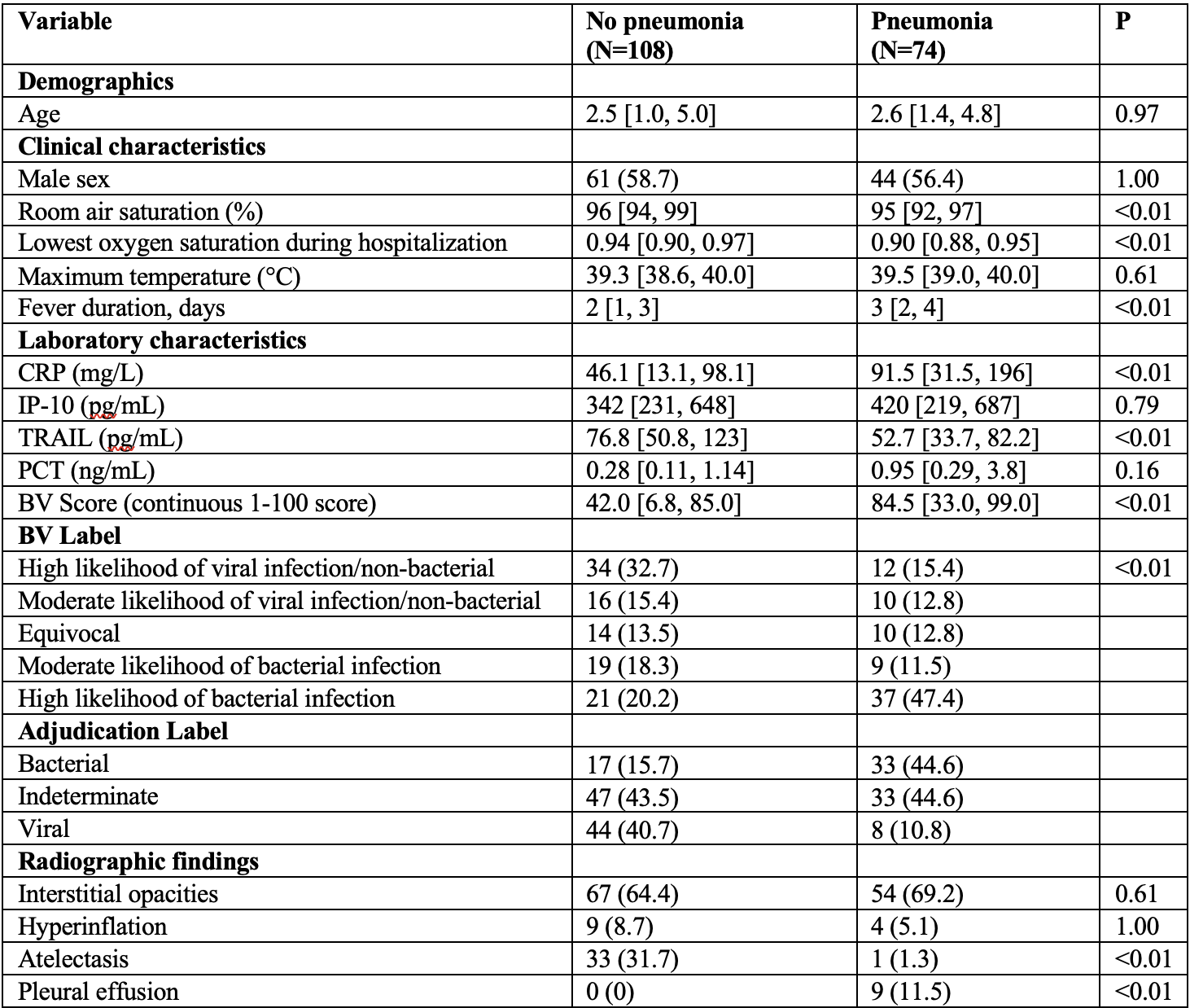
Design/Methods: We performed a secondary analysis of data from a multicenter prospective study, including children 90 days to 18 years presenting to the emergency department with fever who had chest radiography performed. Our outcome was radiographic pneumonia, determined by radiologist adjudication. We evaluated the association of the MeMed BV test with our outcome in isolation and after adjusting for age, room air oxygen saturation, maximum temperature, and fever duration in logistic regression models. We described clinical outcomes stratified by radiographic findings and BV results.
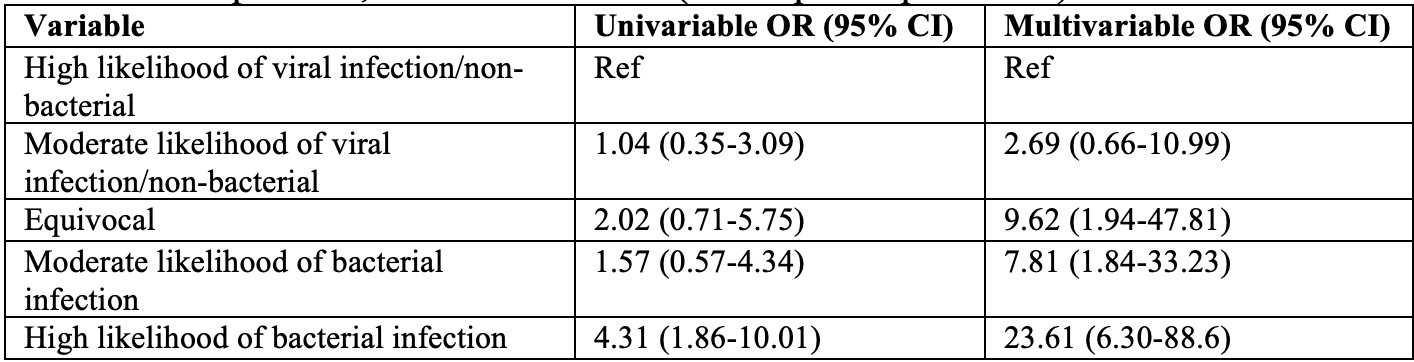
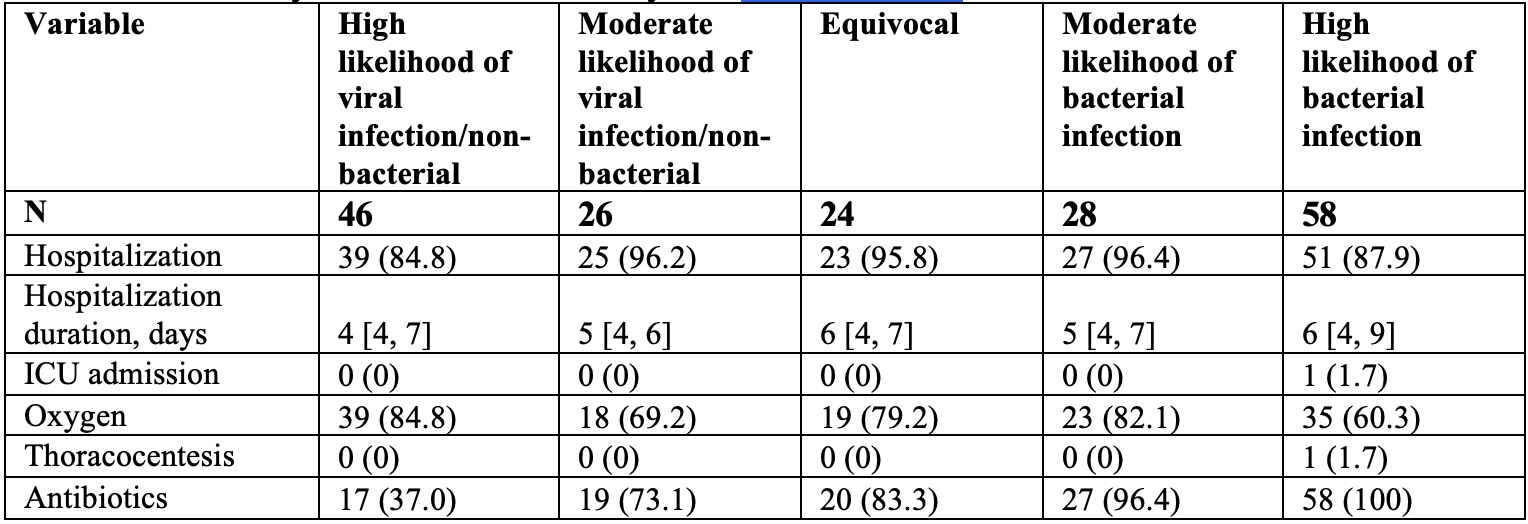
Results: Of 206 children, 74 (41%) had radiographic pneumonia (Table 1). Among children with a high likelihood of having viral illness by BV score (n=46), 26% had radiographic pneumonia; this increased to 60% among those with a high likelihood of bacterial infection (n=58). In univariable analysis, a BV test indicating the highest likelihood of bacterial infection had 4.31 higher odds (95% confidence interval [CI] 1.86-10.01) of radiographic pneumonia; this increased to 23.61 (95% CI 6.30-88.6) in adjusted models (Table 2). Antibiotic use was lower among those with a high likelihood of viral infection, and use of oxygen was lower among those with a higher likelihood of bacterial infection (Table 3).
Conclusion(s): Performance of the BV test was associated with the presence of radiographic pneumonia in children in multivariable models. The BV test did not clearly characterize disease acuity among the secondary outcomes studied. Our findings are supportive of the BV test to identify pediatric pneumonia in children, with further research needed to develop and validate multivariable models incorporating this assay.