Emergency Medicine
Session: Emergency Medicine 5: Sepsis
123 - A Simple Vital Signs-Based Tool for Early Identification of Pediatric Septic Shock
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 123
Publication Number: 123.1630
Publication Number: 123.1630

Nathan Georgette, MD (he/him/his)
Fellow
Boston Children's Hospital
Brookline, Massachusetts, United States
Presenting Author(s)
Background: The temperature- and age-adjusted mean shock index (TAMSI) shows promise for identifying pediatric septic shock but has sub-optimal sensitivity.
Objective: We hypothesized that incorporating respiratory rate (RR) would enhance TAMSI’s sensitivity for incipient shock.
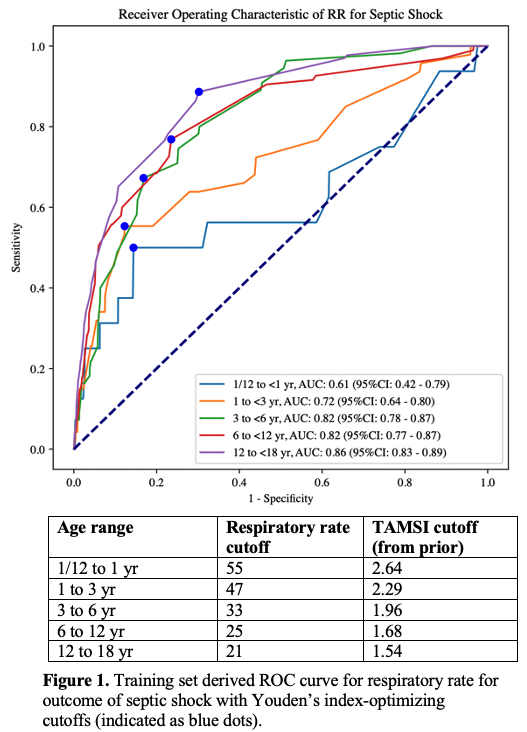
Design/Methods: We analyzed a retrospective cohort of children aged 1 month to < 18 years presenting to a single emergency department (ED) with suspected infection over a 10-year period. TAMSI=[HR-10*(T-37)]/MAP had been previously defined with this cohort’s training set. We defined a positive “TAMSIrr” as a positive TAMSI or an elevated RR. The primary outcome was septic shock, defined as IV vasoactive requirement in setting of suspected infection within 24 hours of ED arrival. The secondary outcome was the “Sepsis-3” consensus definition for septic shock: a lactate>2.0 mg/dL in addition to the criteria above. Missing lactates were assumed normal. In the two-thirds training dataset, we determined an optimal RR cutoff for each age group with Youden’s index. In the one-third validation dataset, we calculated test characteristics for TAMSIrr and compared them to those of the TAMSI and the Pediatric Advanced Life Support (PALS) tachycardia, systolic hypotension, or tachypnea cutoffs.
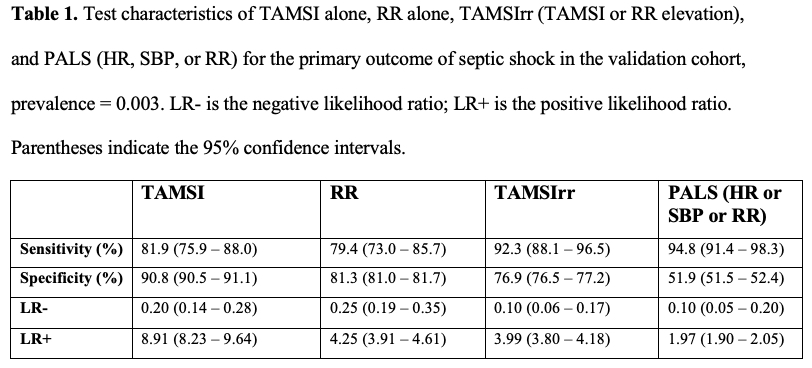
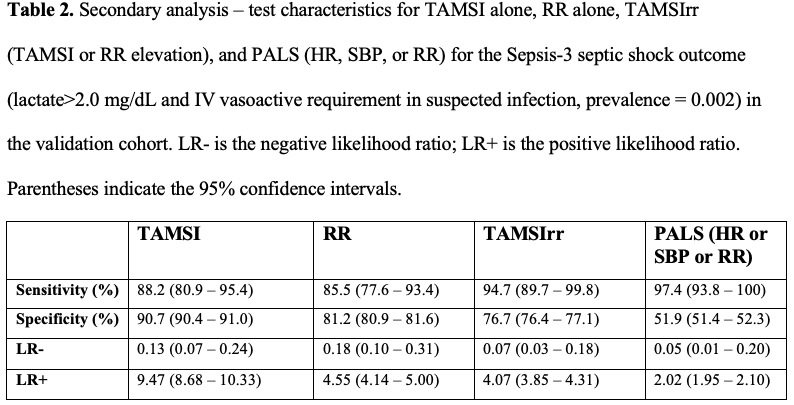
Results: 141,510 encounters were included, of which 508 (0.4%) met the septic shock outcome. RR cutoffs for septic shock were derived in the training dataset (Figure 1). In the validation dataset, for the primary outcome of septic shock, TAMSIrr achieved a sensitivity of 92.3% (95%CI: 88.1–96.5%) and specificity of 76.9% (95%CI: 76.5–77.2%); in comparison, TAMSI achieved a lower sensitivity and higher specificity whereas PALS yielded a similar sensitivity and markedly lower specificity (Table 1). The median lead time from TAMSIrr positivity to start of IV vasoactive was 3.5 hours (IQR: 2.0–6.5) versus 2.8 hours (IQR: 1.4–6.1) for TAMSI. Lactate was measured in 3,597 (2.5%) encounters; 232 (0.2%) met the Sepsis-3 septic shock outcome. The addition of the elevated lactate to the septic shock outcome confirmed the findings from the primary outcome analysis (Table 2).
Conclusion(s): The TAMSIrr is a novel, vital signs-based tool that improves upon PALS specificity for the identification of pediatric septic shock. For both septic shock definitions, TAMSIrr improves upon TAMSI’s sensitivity at the cost of decreased specificity. TAMSIrr’s increased sensitivity and earlier detection may enhance its potential as a screening tool for septic shock. With prospective and multi-center assessment, TAMSIrr could be incorporated into ED septic shock screening tools for children.