Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 1
357 - Outpatient Antimicrobial Stewardship Program Pilot: Targeting Pediatric Healthcare Providers in the Community
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 357
Publication Number: 357.1743
Publication Number: 357.1743

Ilana Waynik, MD (she/her/hers)
Pediatric Hospitalist, Director Clinical Effectiveness
Connecticut Children's
West Hartford, Connecticut, United States
Presenting Author(s)
Background: Inpatient antimicrobial stewardship programs (ASP) have a successful history of reducing inappropriate use of antibiotics. However, 80% of all antibiotics are prescribed in outpatient settings, and various studies have demonstrated up to 76% of outpatient antibiotic prescriptions are inappropriate. The Centers for Disease Control and Prevention published the Core Elements of Outpatient Stewardship in 2016 in response, but limited success was achieved in improvement of outpatient antimicrobial stewardship.
Objective: The aim of this pilot outpatient quality improvement ASP project is to reduce the inappropriate use of antibiotics for 5 common infections [acute otitis media, streptococcal pharyngitis, community acquired pneumonia (CAP), skin and soft tissue infection, urinary tract infection] in 4 Connecticut (CT) Children’s Care Network practices by September 2023.
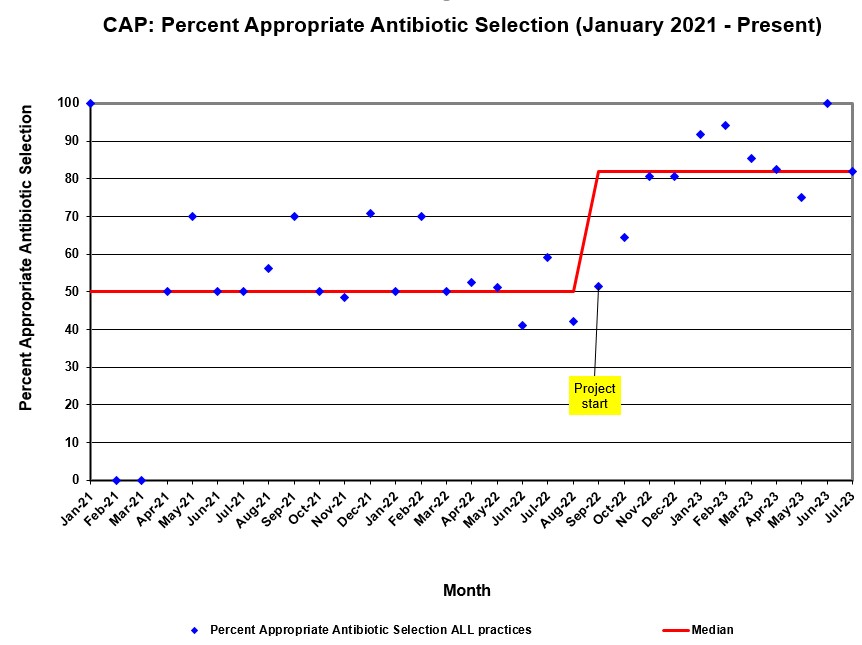
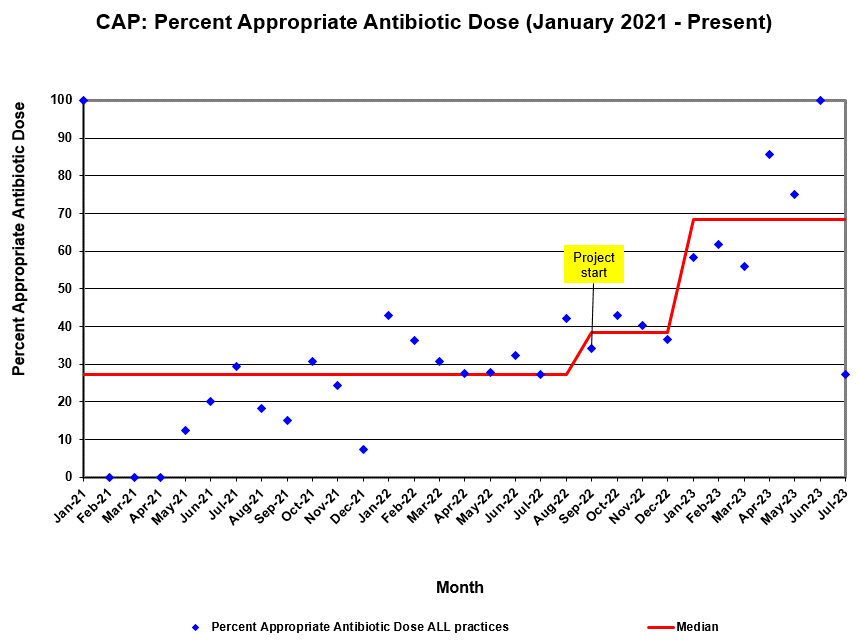
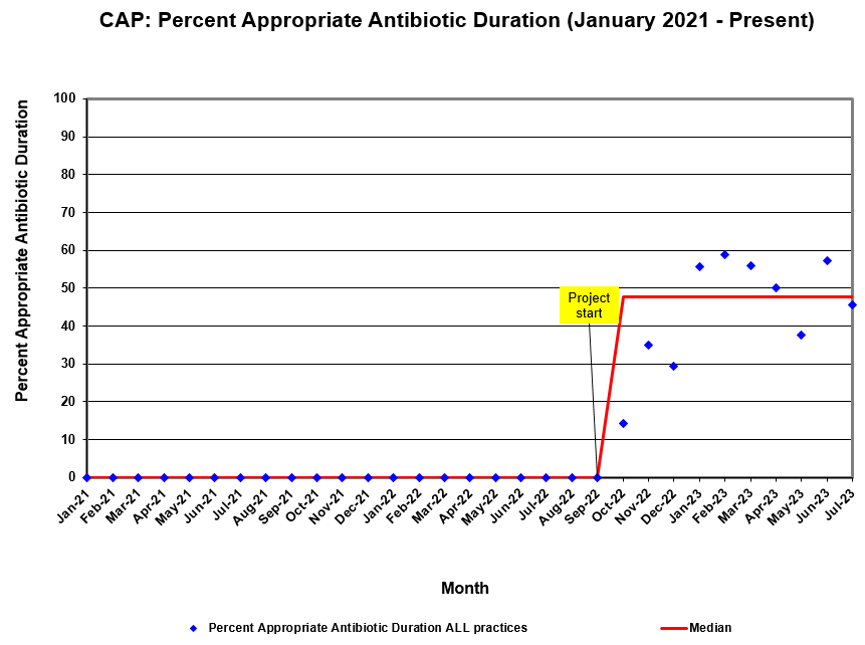
Design/Methods: Quality metrics (antibiotic selection, dose, and duration) were collected monthly utilizing a web-based central reporting solution. Baseline data was captured for a year prior to project initiation allowing each practice to develop individual SMART aims. Metrics were tracked for significant change on run charts for both individual and combined practices. Run charts were annotated with interventions and distributed to the participating practices on a monthly basis.
The following interventions were implemented: in-person and online education that included antibiotic prescribing recommendations and quality improvement training focused on PDSA methodology; distribution of visual aids; tutorial on use of Firstline, an evidence-based clinical decision point-of-care antimicrobial prescribing tool; direct access to project leaders, including ASP clinicians, for questions; continual review of monthly metrics.
Results: Current all-practice, all-condition data demonstrated improvement in overall appropriate antibiotic use, with significant improvement in median of antibiotic selection (76% - 90%), dose (29% - 48%), and duration (61% - 81%). CAP metrics for all practices combined demonstrate significant improvement in median of antibiotic selection (50% - 82%), dose (27% - 68%), and duration (0% - 47%).
Conclusion(s): This pilot outpatient ASP project has proved an effective model for improving appropriate antibiotic usage. Participating practices will continue to work through their current SMART aims. Additionally, several practices are actively working on higher reliability interventions, such as EHR note templates and order sets. Our plan is to expand this pilot to determine feasibility of scaling to all of CT Children’s Care Network.