Emergency Medicine
Session: Emergency Medicine 2: Operations
372 - How Super is Supertrack? Improving Flow of Fast Track Patients through a Pediatric Emergency Department
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 372
Publication Number: 372.51
Publication Number: 372.51
- DL
Daniel Lam, MD (he/him/his)
Pediatric Emergency Medicine Fellow
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background: Patient crowding in Pediatric Emergency Departments (EDs) prolongs patient care and decreases patient satisfaction. In 2016, our institution created a rapid assessment “intake” space, where low acuity patients were evaluated and then either discharged home or moved to an ED bed for further care. Those moved to the ED but who were anticipated to require no more than one hour of additional care were identified as fast track patients and given a “Supertrack” designation to expedite care in the ED. Prior to this project, only 17% of Supertrack patients were discharged within one hour of receiving their ED bed.
Objective: Our aim was to improve the percentage of Supertrack patients discharged within one hour of receiving their ED bed from 17% to 50% over a 10-month study period.
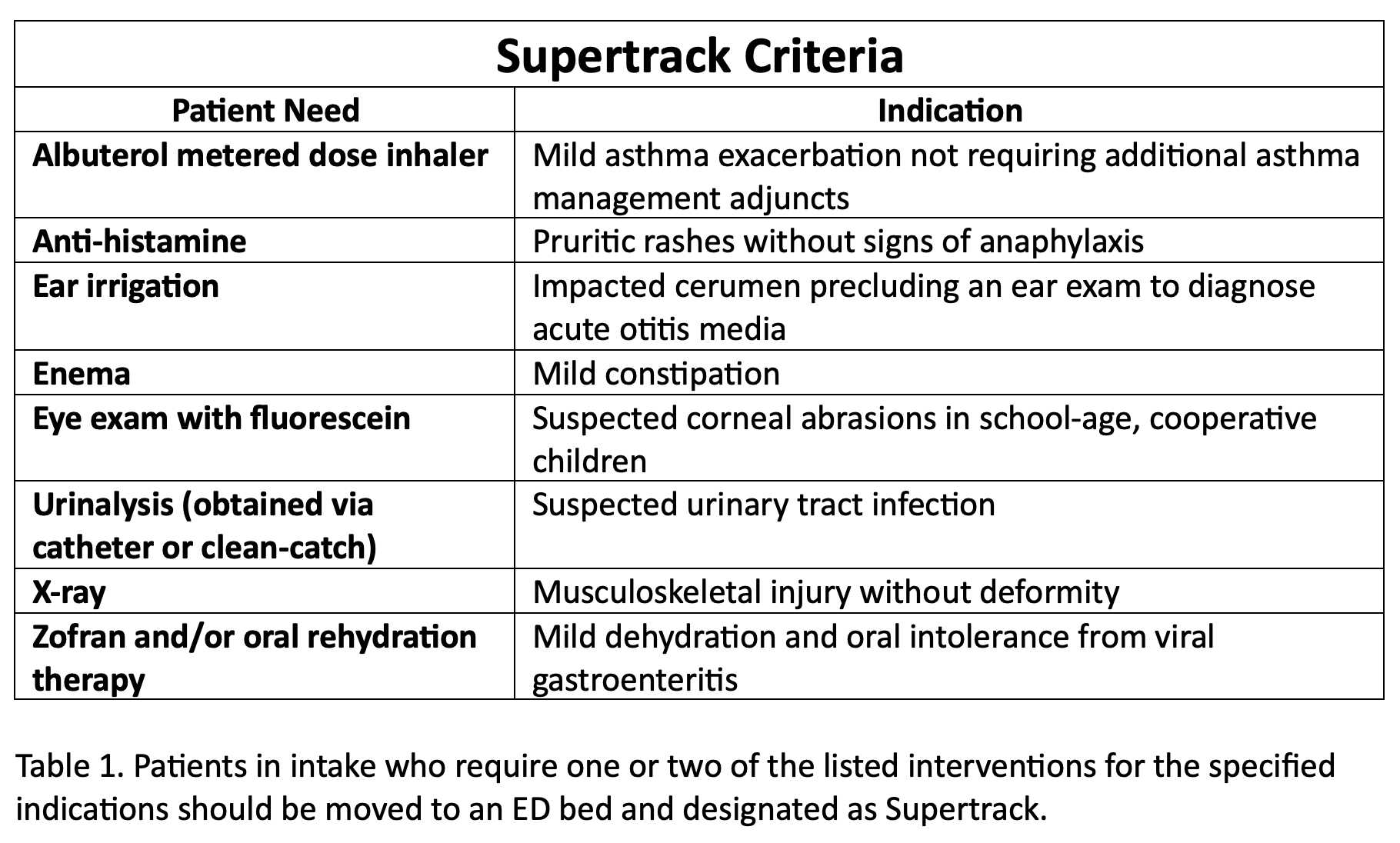
Design/Methods: Our primary outcome measure was the percentage of Supertrack patients discharged within one hour of receiving their main ED bed. Process measures included adherence to Supertrack criteria and time to ED provider assignment. Our balancing measure was return visits for Supertrack patients within 72 hours of discharge. Interventions occurred over four PDSA cycles and included intervention-based criteria for the Supertrack designation (Table 1), email reminders and monthly project updates for ED staff, live alerts by QI Clinical Champions, intake provider huddles, and documentation prompts for intake scribes.
Results: The percentage of Supertrack patients discharged within one hour of their ED bed assignment increased from 17% to 27% (Fig. 1). We observed special cause variation during an unexpected respiratory surge as well as at the onset of our live alerts by QI Clinical Champions. Adherence to Supertrack criteria by intake providers was 55%. There was no significant change to the rate of ED return visits within 72 hours.
Conclusion(s): Our project increased the number of Supertrack patients discharged within their anticipated timeframe. Live alerts from QI Clinical Champions had the largest effect on our outcome measure but were difficult to sustain. Limitations included an unexpected surge in respiratory illnesses at the onset of this study. Difficulties with forming a physical Supertrack area with a dedicated provider role for these patients contributed to a modest improvement to our outcome measure. Our findings are useful to institutions seeking to develop their own fast track models despite limited space and staffing availability.
.png)
