Neonatology
Session: Neonatal Neurology 2: Clinical
21 - Individualized Neuroprognostication in Neonates with Hypoxic-Ischemic Encephalopathy by Combining Clinical Factors, Neurophysiology, and Neuroimaging
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 21
Publication Number: 21.379
Publication Number: 21.379

Mehmet N. Cizmeci, MD, PhD (he/him/his)
Neonatologist, Associate Professor of Pediatrics
University of Toronto Temerty Faculty of Medicine
University of Toronto
Toronto, Ontario, Canada
Presenting Author(s)
Background: .
Objective: We aimed to individualize neuroprognostication in neonates with hypoxic-ischemic encephalopathy (HIE) treated with therapeutic hypothermia (TH) using clinical factors, amplitude-integrated EEG (aEEG) features, and brain MRI injury patterns.
Design/Methods: A retrospective multicenter study of 153 infants treated with TH for HIE between 2010-2020 was conducted. Brain MRI (median [interquartile range] day 6 [2-10]) was scored by two independent investigators using the Rutherford scoring system. Neuroimaging patterns were categorized as normal, basal ganglia/thalami-predominant, white matter/watershed-predominant, and near-total injury. The severity of HIE on presentation using the Thompson score, aEEG background pattern, and the number of seizures were assessed. Prognostication for each domain was categorized as highly unlikely, possible, probable, or highly likely based on the previous research by Martinez-Biarge et al. A consensus agreement was used for outcome prediction for each developmental domain. Outcomes were predicted separately for mortality, cerebral palsy (CP) and severity, cognitive delay, post-neonatal epilepsy, cerebral visual impairment (CVI), and oro-motor problems requiring prolonged gavage feeding. Neurodevelopment was assessed at 2 years by experts blinded to the MRI scoring and prognostication given.
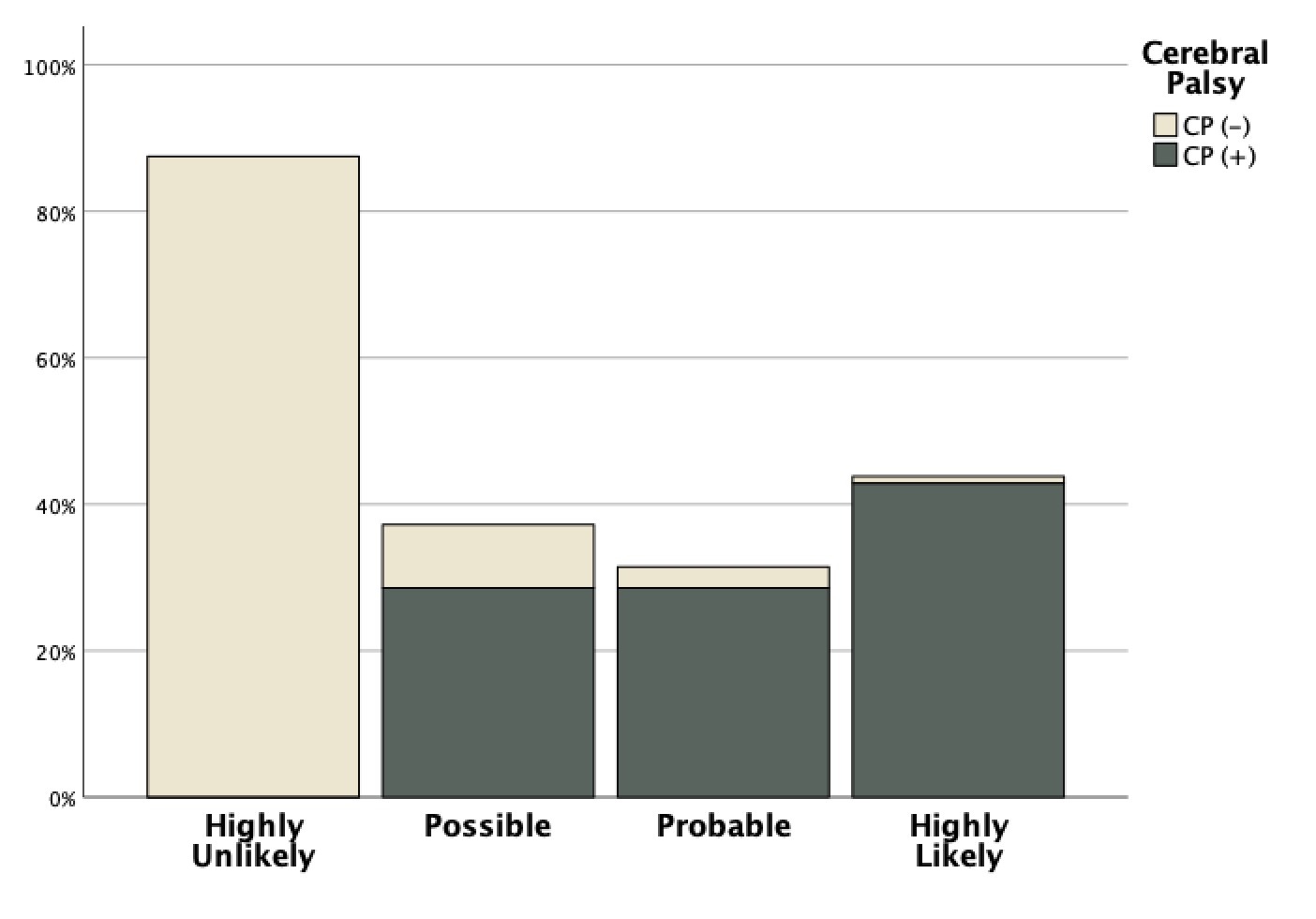
Results: On presentation, the median (IQR) Thompson score was 10 (8-12) and 65 (43%) infants had suppressed background patterns on aEEG. Electrographic seizures were seen in 91 (60%) infants of which 38 (25%) were repetitive and 15 (10%) status epilepticus requiring 2 or more anti-seizure medications. Overall, 27 (18%) infants died and the prediction of redirection of care achieved 95% accuracy, sensitivity, and specificity. The predictive category of CP was accurate for 80% of the survivors. No infants in the highly unlikely category developed CP and 90% in the highly likely category did. For the cognitive outcome on the Bayley-III test, the predictive category was accurate in 49% of the infants, differed by 1 category in 33%, by 2 categories in 13% and by 3 in 3%. When cognitive delay was predicted as highly unlikely, 92% did not develop cognitive delay whereas when this was considered highly likely 100% developed cognitive delay. The predictive category of epilepsy, CVI or feeding problems was accurate in 77%, 84%, and 83% respectively.
Conclusion(s): Individualized categorical neuroprognostication in neonates with HIE by combining clinical factors, neurophysiology, and brain MRI is feasible and reliable for most neurodevelopmental domains.