Neonatology
Session: Neonatal General 6: POCUS, Technology in NICU
151 - Evaluation of an Optical Coherence Tomography Device for Real-Time Infant Nasogastric Tube Placement: A Rabbit Model
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 151
Publication Number: 151.2022
Publication Number: 151.2022

Amanda E. Winkler, MD (she/her/hers)
Fellow
Boston Children's Hospital
Belmont, Massachusetts, United States
Presenting Author(s)
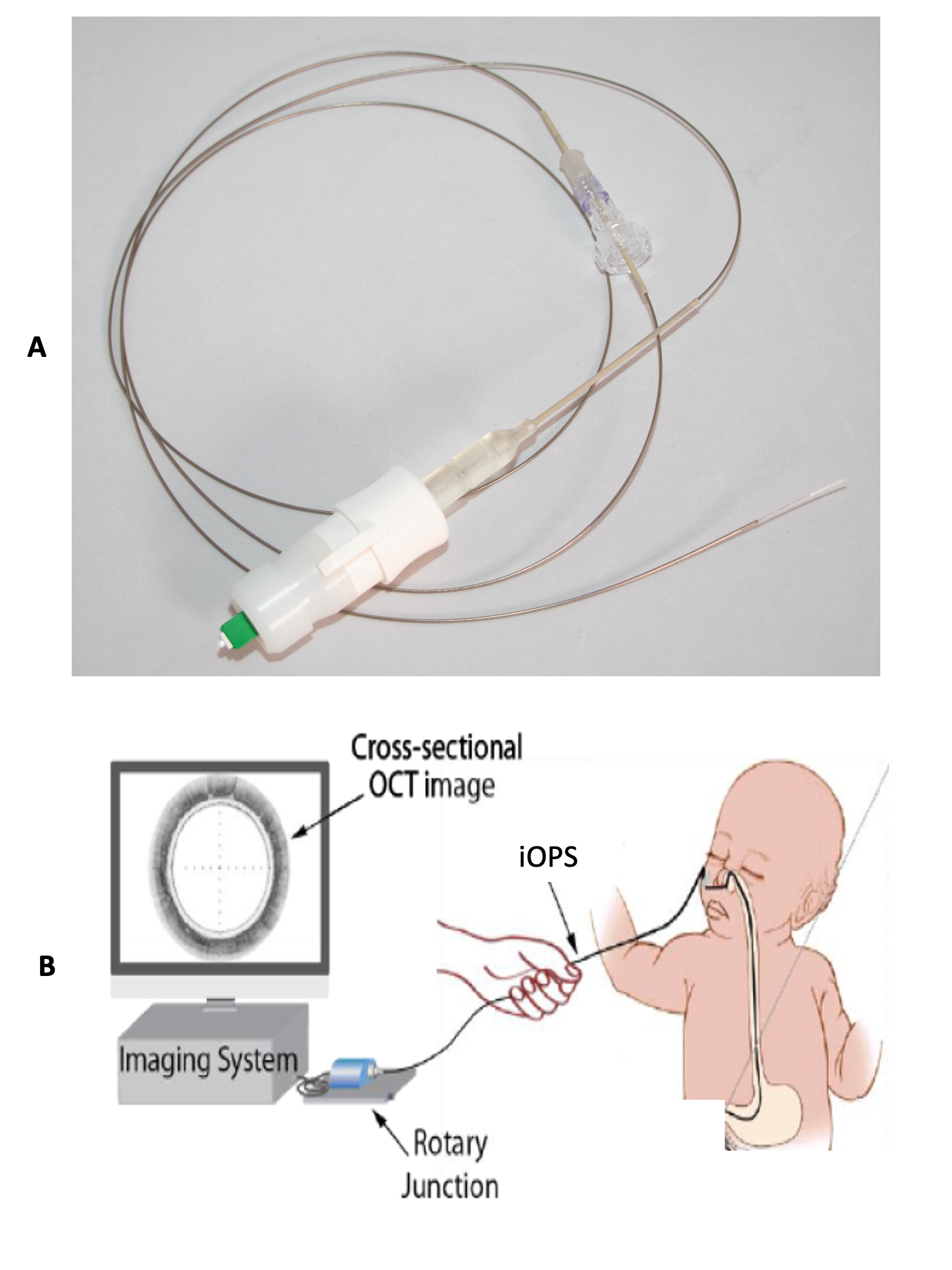
Background: Optical coherence tomography (OCT) is a high spatial-resolution, cross-sectional, laser imaging modality. We have developed a novel 1.125 mm diameter, flexible OCT imaging device titled the Infant Optical Probe Subsystem (iOPS) to obtain detailed images of subsurface structures in the upper gastrointestinal tract. Nasogastric (NG) tube placement is an instrumental procedure in the care of critically ill infants used for enteral access and gastric decompression. Although NG tube placement is a common procedure, the risk of misplacement or perforation remains significant. While data is limited, prior studies have shown an incidence of NG tube misplacement, including esophageal, post-pyloric, or extra-gastrointestinal, as high as 59% in the ill infant population. When placed into the lumen of a clinical nasogastric (NG) tube, the iOPS is designed to provide real-time confirmation of NG tube placement.
Objective: To evaluate the feasibility of the iOPS to provide real-time OCT confirmation of nasogastric tube placement in a rabbit model to simulate neonatal placement.
Design/Methods: The iOPS device is comprised of a 0.5mm diameter optical fiber encapsulated within a 2m-long 3.5 Fr rotatable sheath (Fig.1). The optical fiber terminates in a lens the redirects coherent light towards the abdominal wall while the sheath rotates to obtain circumferential images. To simulate clinical NG tube placement, the iOPS was pre-threaded into a 6.5 Fr polyurethane NG tube and orally inserted into a deceased New Zealand White rabbit model due to limitations in nostril size. OCT images were captured from oral insertion to NG tube termination in the gastric body and during subsequent removal through the lumen, leaving the NG tube in situ.
Results: We used the iOPS to obtain detailed OCT endomicroscopy images of the esophagus and stomach in a deceased rabbit model, with anatomical differentiation between organ-specific morphology (Fig.2). There was no evidence of perforation on post-procedure gross tissue examination. Histology of rabbit tissue, compared to standardized values in infants < 1 year of age, including esophageal diameter (5 mm vs 8 mm), gastric mucosal thickness (1.2 mm vs 1 mm) and small bowel diameter (8.5 mm vs 15 mm), respectively, were comparable.
Conclusion(s): A rabbit model evaluating gastrointestinal OCT deployment demonstrates the feasibility of using the iOPS for evaluation of esophageal and gastric mucosa tissue morphology for real-time confirmation of nasogastric tube placement.
.png)
