Neonatology
Session: Neonatal Neurology 1: Clinical
5 - Evolution of Hypoxic-Ischemic encephalopathy: Role of serial Sarnat exams in first 6 hours of age
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 5
Publication Number: 5.448
Publication Number: 5.448

Daniel D. Sprehe, MD (he/him/his)
Resident Physician
Washington University in St. Louis School of Medicine
St. Louis, Missouri, United States
Presenting Author(s)
Background: Sarnat exams are used to evaluate infants eligible for treatment with Therapeutic Hypothermia (TH). It is unclear how serial Sarnat exams within the 6-hour TH window affect decisions to provide TH in infants with moderate or severe Hypoxic-Ischemic Encephalopathy (HIE).
Objective: To evaluate usefulness of serial Sarnat exams in newborn infants after birth and decision to treat with or without TH.
Design/Methods: Infants ≥ 35 weeks gestational age eligible for TH (≥35 weeks, acidosis, resuscitation, perinatal events) were evaluated with Sarnat exams, either single or serially within 6 hours of birth. Maternal and infant clinical and demographic factors data including detailed Sarnat exam in all 6 categories (level of consciousness, spontaneous activity, tone, posture autonomic responses and primitive reflexes, and categorized into normal, mild, moderate or severe) at each exam were collected. Infants were stratified into TH and non-TH groups. Chi-square and t-tests were used for group differences. CART (qualitative) analyses were used to determine exam category that led to TH or not.
Results: 92 infants with complete Sarnat exam were identified of whom 68 (74%) received TH and 24 (26%) did not. 59 (64%), 39 (43%), 16 (17%), 4 (4%) and 3 (3%) infants had 1 to 5 exams respectively.
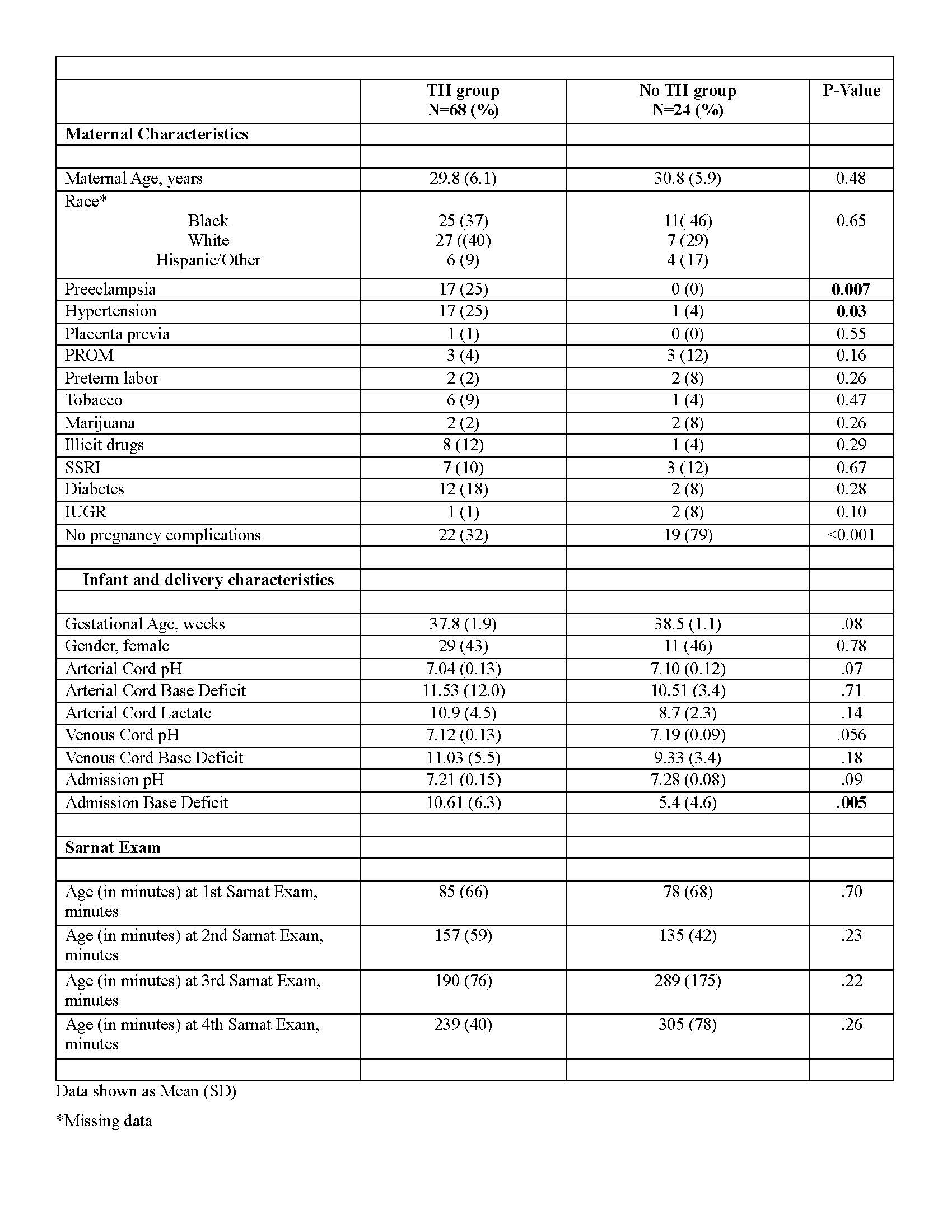
Clinical and demographic differences in infants with or without TH are shown in Table 1. Maternal hypertension, preeclampsia were more common in TH group, while absence of pregnancy complications more common in no-TH group. Infant characteristics and age at exam were similar in the two groups. 56/59 (95%) infants with one exam, 18/39 (46%) with 2 exams, 8/16 (50%) with 3 exams, 4/7 (57%) with 4 exams, and 2/3 (67%) with 5 exams were treated with TH.
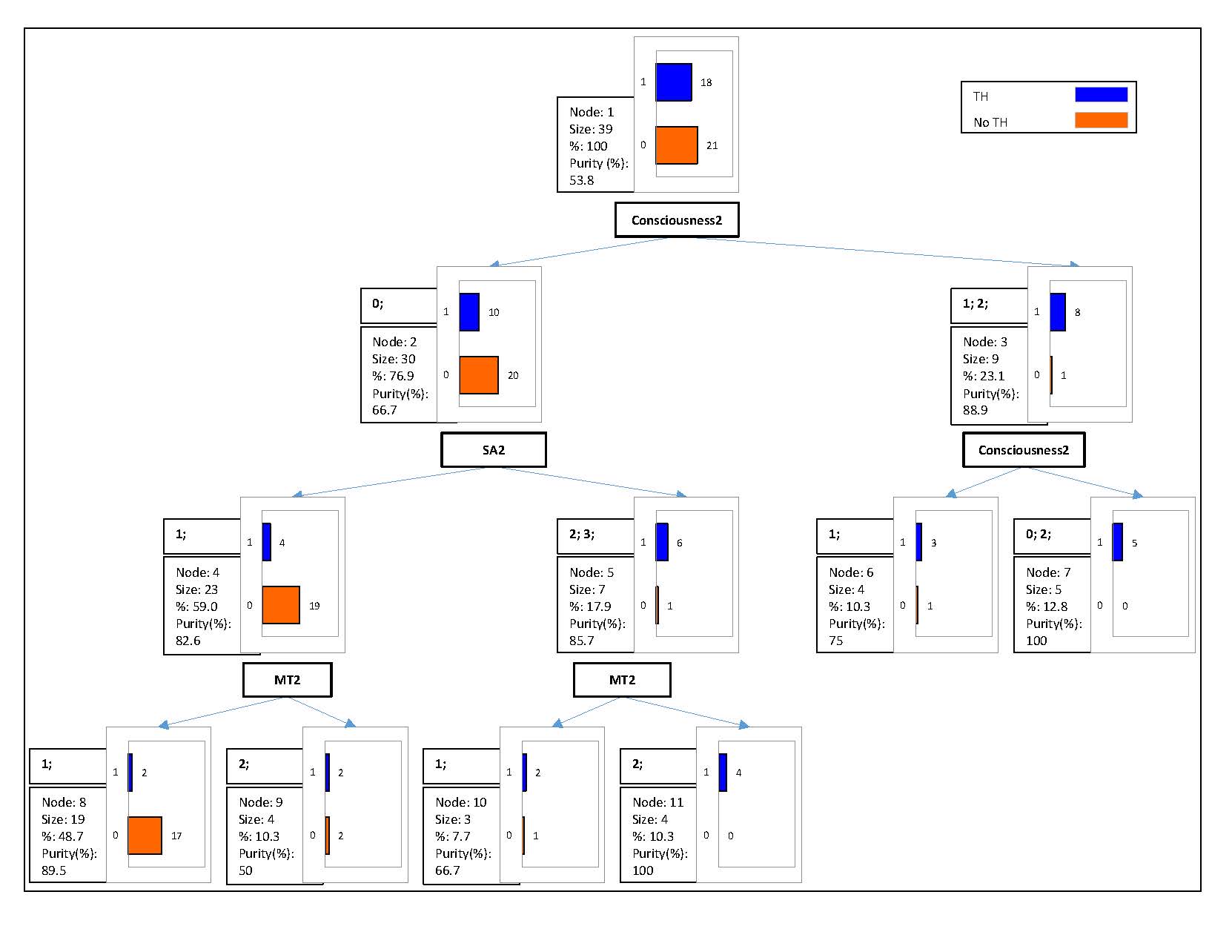
At the first exam, abnormal levels of consciousness, muscle tone and suck reflex were noted in infants treated with TH (Figure 1). When level of consciousness was normal at first exam, only 15% went on to be cooled subsequently. At the second exam, level of consciousness, spontaneous activity and muscle tone were drivers for treating with TH (Figure 2). When level of consciousness was normal at second exam, only 10.3% of infants were cooled. At the third exam, abnormal level of consciousness, muscle tone and an abnormal Moro’s reflex were determinants for TH. If consciousness was normal at 3rd exam, then 19% of infants were cooled.
Conclusion(s): Decision for TH was made in 74% of patients. In infants with >1 exam, between 46%-67% received TH, highlighting that serial exams are important to identify infants eligible for TH within 6 hour window.
.jpg)