Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 6
51 - Improving Pediatric Rapid Response Communication
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 51
Publication Number: 51.2944
Publication Number: 51.2944
Arshiya Ahuja, MD (she/her/hers)
Assistant Professor of Pediatrics
University of North Carolina
Chapel Hill, North Carolina, United States
Presenting Author(s)
Background: Rapid response systems are vital to the early identification and rescue of clinically deteriorating patients and can reduce rates of inpatient non-intensive care unit cardiac arrest and overall in-hospital mortality. Effective rapid response systems require teamwork and communication, without which results in substandard patient care and worse outcomes. Among 90 pediatric nurses and providers at our institution, only 28% felt that communication was clear and effective the majority of the time and only 25% knew the role of other team members during the rapid response a majority of the time.
Objective: The global aim was to improve communication, efficiency, and effectiveness of the pediatric rapid response process. The SMART aim was to implement a communication bundle to enhance clarity and optimize teamwork during rapid response events, with a compliance goal of 60% by October 2023.
Design/Methods: The project utilized the Model for Improvement. We established a multidisciplinary team including rapid response nurses, floor and ICU nurses, hospitalists, residents, ICU physicians, respiratory therapists and pharmacists. Nurses and providers completed a pre-survey to help identify areas for improvement. Input was provided by the family advisory committee. Rapid response role badges were created to better identify team members and reduce unneeded personnel. A communication bundle was implemented which included a time out for introductions, SBAR (situation, background, assessment, recommendation), and debrief. Patients and families were encouraged to participate in the communication bundle components. Education via email, oral presentations and simulation was completed. Tip sheets for reminders for use were provided. Data was collected through online surveys completed after each rapid response.
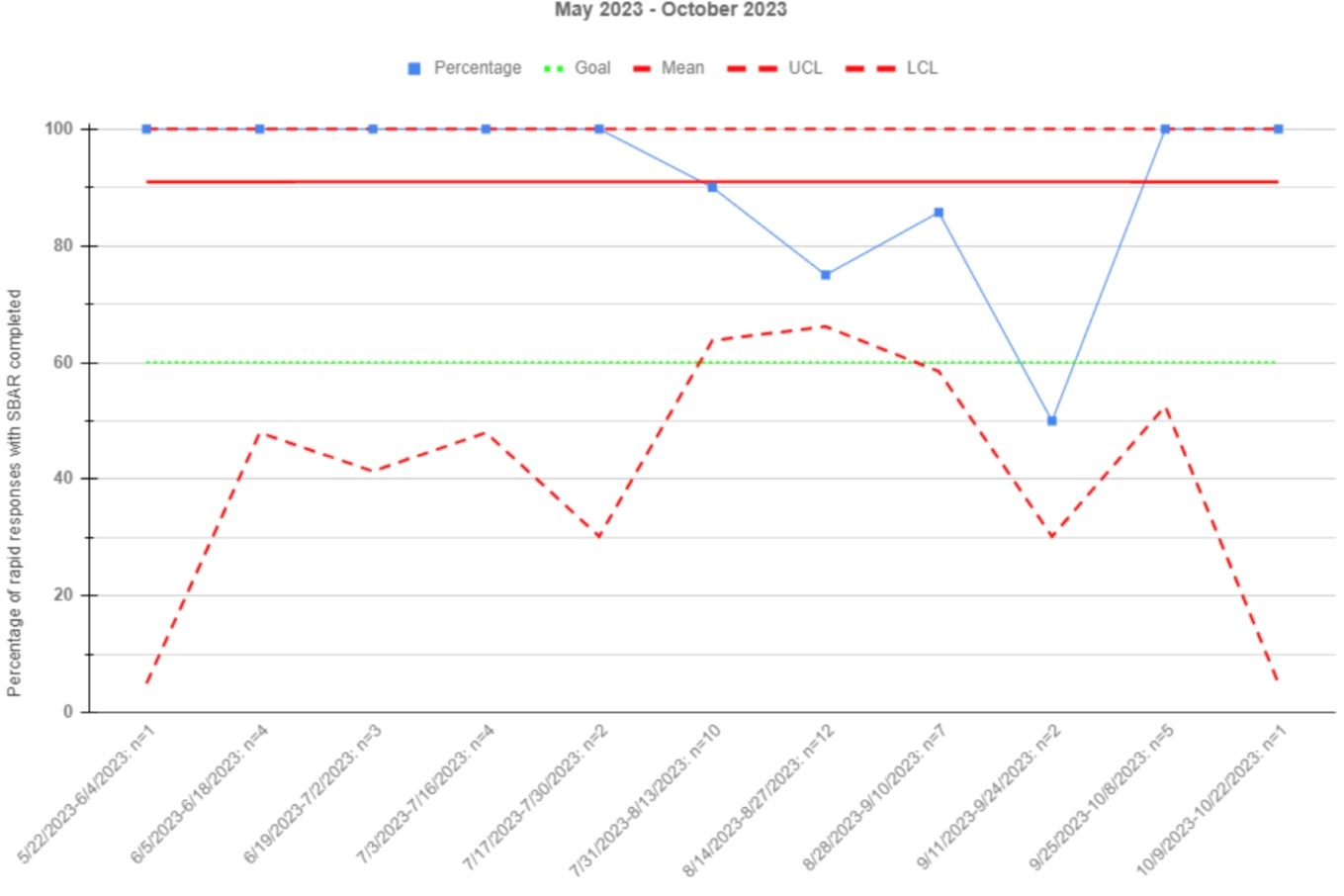
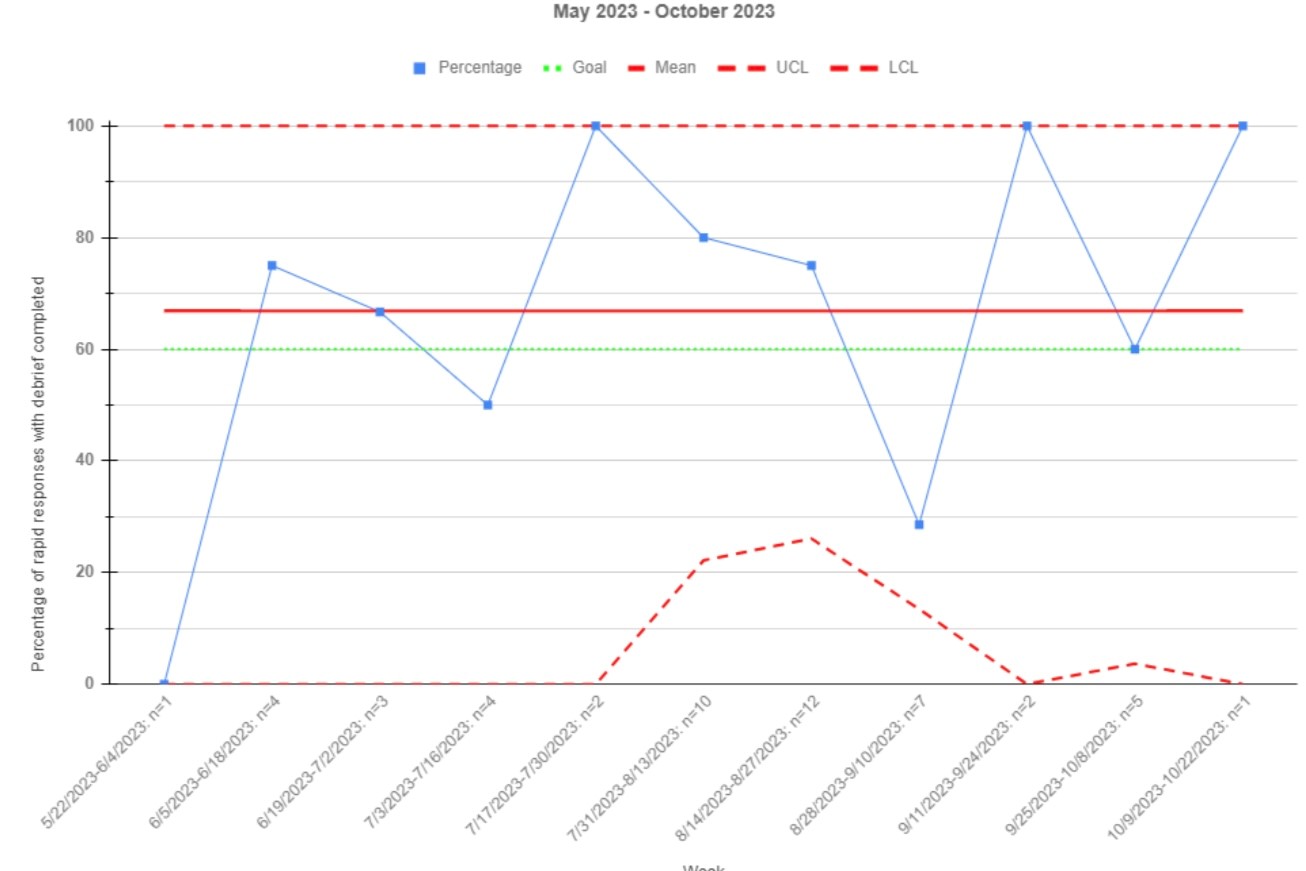
Results: The proportion of rapid responses with all components of the communication bundle increased from 0% to a mean of 60% among rapid responses with completed surveys. Surveys were completed a mean of 50% of the time. The mean proportion of rapid responses with introductions was 76%, with SBARS was 91%, with review of the plan of care 99%, and with debriefs was 67%.
Conclusion(s): Utilizing the principle of alignment with strong nursing leadership support and a multidisciplinary team we have been able to achieve culture and process changes and improved communication during pediatric rapid responses with the use of the communication bundle. PDSAs are ongoing to target survey completion, SBAR clarity, and debriefs.
.jpg)
