Neonatology
Session: Neonatal-Perinatal Health Care Delivery: Practices and Procedures 3
472 - Discharge Timing Among a Contemporary Cohort of Infants Born 22-34 Weeks of Gestation
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 472
Publication Number: 472.2943
Publication Number: 472.2943

Sara C. Handley, MD, MSCE (she/her/hers)
Assistant Professor of Pediatrics
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Prior publications show that NICU hospitalizations are increasing in length. However, such studies do not include all extremely preterm ( < 24 weeks) nor moderately preterm infants (30-34 weeks). Given the increase in intensive care initiation for infants < 24 weeks and evolving practices for moderately preterm infants, it is essential to understand current NICU utilization patterns for adequate resource deployment.
Objective: To evaluate the discharge characteristics of post menstrual age (PMA) and weight among preterm neonates (22 to 33 weeks’ gestation) from 2018 through 2022 in a national data source.
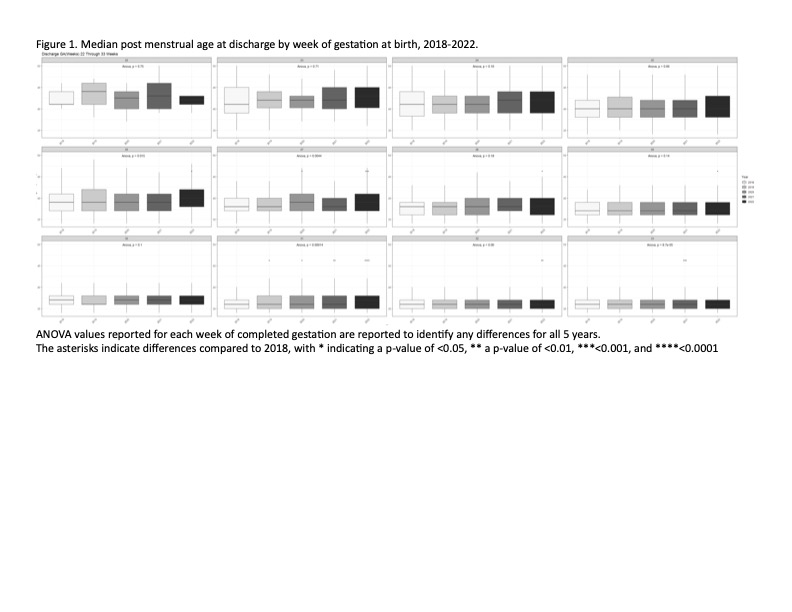
Design/Methods: Retrospective cohort study utilizing Epic Systems’ Cosmos research database, which uses aggregated electronic health record data from over 1,200 hospitals. Infants 22+0–33+6 weeks’ gestation born from 1/1/2018 to 12/31/2022 who were not transferred and survived to hospital discharge were included. The PMA and weight at discharge were examined annually and stratified by completed week of gestation. Differences between years were assessed using ANOVA with adjustment for multiple comparisons referencing 2018.
Results: There were 37,671 eligible infants, with a median birth gestational age of 32 weeks’ gestation (IQR 29-33) and birth weight of 1710 grams (IQR 1320-2070). The median PMA at discharge did not change for infants born from 22 to 25 weeks between 2018 and 2022. However, by 2022, the median PMA at discharge increased by 1 week for infants born between 26 and 28 weeks, with discharge in 2022 at a median PMA of 40, 39, and 38 weeks, respectively. Changes in median PMA at discharge varied among infants born 29-33 weeks (Figure 1). Trends in weight at discharge paralleled these findings (Figure 2).
Conclusion(s): These data show that PMA at discharge for the most extremely preterm infants has not changed in recent years, yet is increasing among the very and some moderate preterm infant populations. While these findings suggest stable resource utilization for the most preterm infants, increasing PMA at discharge among other preterm populations is a noteworthy trend. Further analysis of variations in NICU care and discharge timing across hospitals may reveal more safe and efficient discharge practices for preterm infants.
.jpg)
