Neonatology
Session: Neonatal-Perinatal Health Care Delivery: Practices and Procedures 2
457 - The Impact of Electronic Documentation on Documenting Nurse Workload during Delivery Room Resuscitation
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 457
Publication Number: 457.2971
Publication Number: 457.2971
- CL
Charis Lim, BPsych(Hons) (she/her/hers)
Clinical Research Coordinator
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
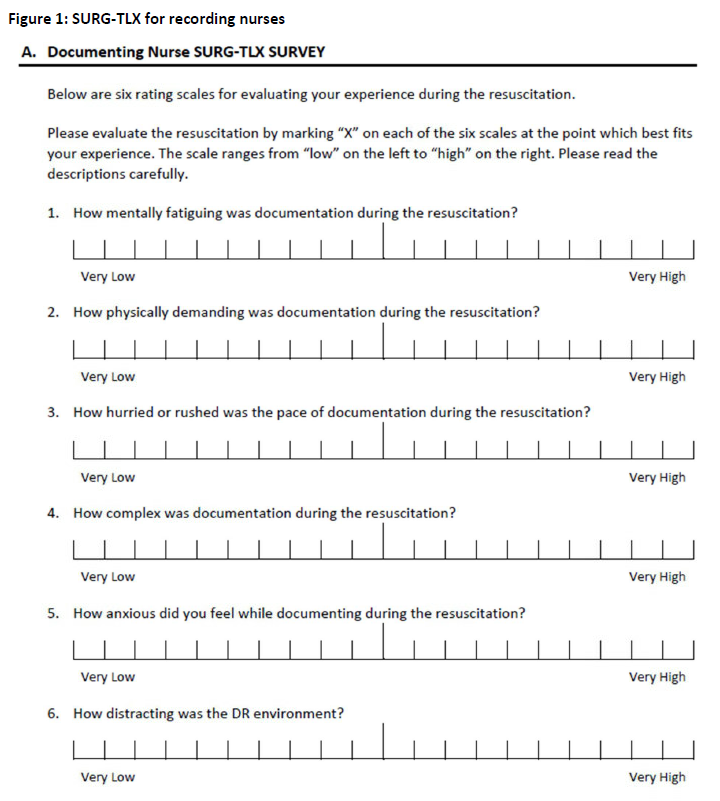
Background: The Surgical Task-Load Index (SURG-TLX), a validated survey for healthcare environments adapted from the NASA Task-Load Index (NASA-TLX), measures provider workload across 6 domains. The Special Delivery Unit (SDU), a delivery room (DR) devoted to neonates with congenital anomalies at the Children’s Hospital of Philadelphia, transitioned from paper to electronic documentation for DR resuscitation. The impact of electronic versus paper documentation on DR nurse workload is unknown.
Objective: To measure the impact of electronic documentation on documenting nurse workload using the SURG-TLX.
Design/Methods: Observational study assessing documenting nurse workload during DR resuscitation across three epochs: (1) paper documentation, (2) transition period and (3) post-electronic documentation. Transition and post epochs were defined by nurse experience with electronic DR documentation < 3 times (transition) and electronic documentation >=3 times (post). Documenting nurses were asked to complete the SURG-TLX (Figure 1) within 3 hours of the resuscitation when a study team member was available. The primary outcome was raw SURG-TLX score (sum across domains, 6-120) and secondary outcomes were subscale scores (1-20). Univariable and multivariable analyses compared primary and secondary outcomes across epochs. Nurse, patient, and resuscitation characteristics associated with raw SURG-TLX score with a p-value < 0.05 were considered for inclusion in multivariable regression.
Results: Between 6/23-10/23, 58 SURG-TLXs were collected. Table 1 shows patient, nurse, and resuscitation characteristics by epoch. In univariable analysis there was no difference in raw SURG-TLX (paper: mean 31.9 (SD 21.5), transition 40.9 (19.3), post 33.3 (17.1), p=0.29) nor subscale scores by epoch. In multivariable analysis including highest level of respiratory support and highest level of vascular access in the DR, there was no difference in raw or subscale SURG-TLX scores between paper and post epochs (Table 2). The transition epoch was associated with an increased raw SURG-TLX score (beta coefficient 12.5 [95% CI 1.3-23.6] p=0.03) and increased situational stress and distractions subscale scores.
Conclusion(s): Transition to DR electronic documentation was associated with a transient, but not sustained, increase in overall workload for documenting nurses in multivariable analysis, which appears to be driven by situational stress and distractions. These findings reinforce the need for adequate planning and training prior to implementation of new processes to minimize learning curve effects.
.png)
.png)
