Mental Health
Session: Mental Health 2
568 - Geospatial Suicide Risk Identification at Children’s Wisconsin Using Inpatient Ask Suicide-Screening Questions (ASQ): Exploring Demographic Disparities and Discharge Outcomes
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 568
Publication Number: 568.1979
Publication Number: 568.1979

Alexandra L. Johnson, BS (she/her/hers)
Medical Student
Medical College of Wisconsin
Milwaukee, Wisconsin, United States
Presenting Author(s)
Background: Suicide rates in America’s youth have become an increasing public health concern and we are in the midst of an adolescent mental health crisis.
Objective: To assess demographics of those screened with the Ask Suicide-Screening Questions (ASQ) and elucidate if this informs discharge disposition.
Design/Methods: Retrospective cohort study of patients aged 10-17 hospitalized for intentional self-harm or suicidal ideation between May 01, 2021, and May 01, 2022. Female and male sex assigned at birth of all races and ethnicities were included. Classification of socioeconomic status (SES) according to zip code was based on the Center for Urban Population Health Milwaukee Health Report.
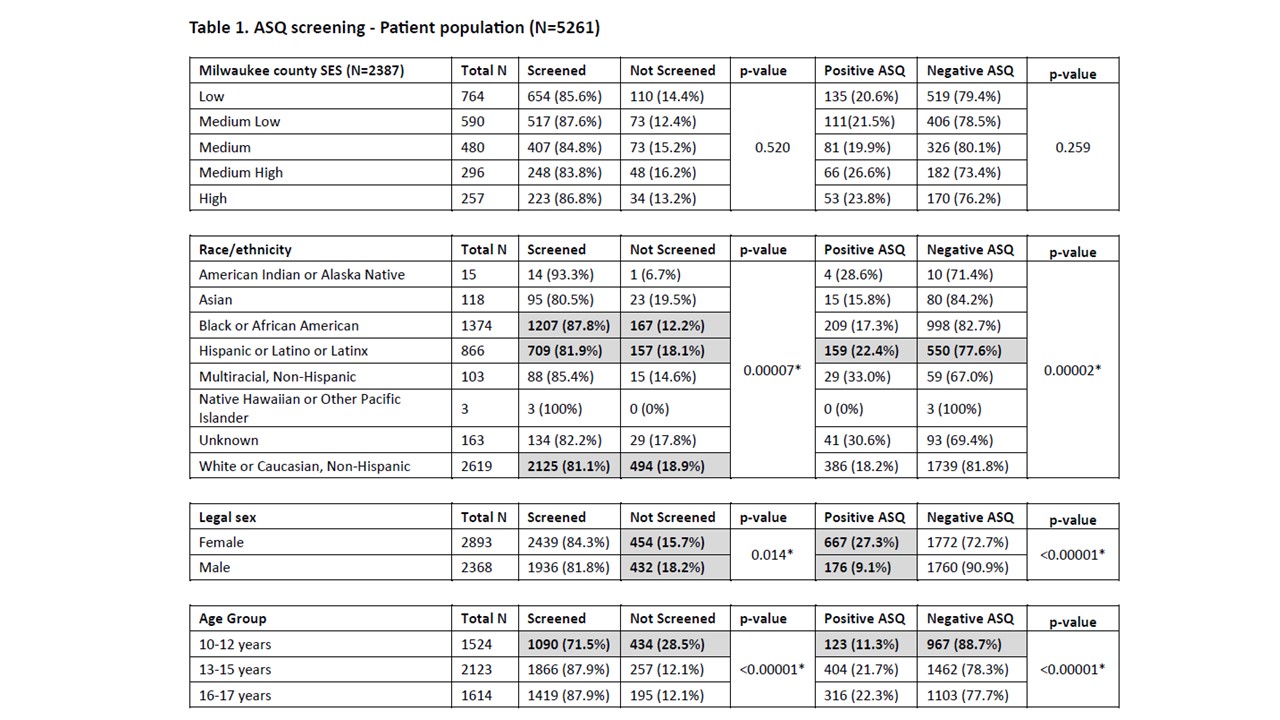
Results: 5,261 patients met our inclusion criteria. 2,387 patients were Milwaukee County residents. Of our total cohort, 4,375 (83.2%) were screened and 843 (19.3%) had a positive result. Acute positive screens represented 22.3% of all positive results. Black or African American (BAA) patients were screened more than other races/ethnicities (87.8%, p = 0.00007). Hispanic, Latino, or Latinx patients were screened the second most frequently (81.9%, p= 0.00007) with more negative results (77.6%, p = 0.00002). Female sex was associated with more positive screens (27.3%, p< 0.00001). Males were screened less than females (18.2%, p = 0.014). Patients aged 10-12 years were screened less than older patients (71.5%, p < 0.00001) and had fewer positive results (88.7%, p< 0.00001) (Table 1). There was no statistically significant difference in discharge location based on acute positive result (p = 0.287) or SES (p = 0.439). Patients with low SES were more commonly discharged home (60.7%, p = 0.439). BAA patients were discharged home more often than to psychiatric facilities (65.1% vs 33.5%, p = 0.00021), compared to White or Caucasian patients (49.7% vs 50%). Patients discharged home were more likely to revisit the emergency department (ED) within 1 week of discharge (6.1%, p = 0.009).
Conclusion(s): Patients discharged home presented to the ED within 1 week of their initial discharge more often than those discharged elsewhere. BAA patients were discharged home more often than to a psychiatric facility. Despite high acuity and increased resource utilization, there was no difference between acute positive results and discharge location. This study offers a perspective on social determinants of health and hospital utilization following a positive suicide screen and demonstrates the importance of cultural awareness and consideration of social determinants when targeting interventions for patients at risk for suicide.