Neonatology
Session: Neonatal/Infant Resuscitation 1
260 - Effect of CPAP interface and pressure in delivery room and NICU
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 260
Publication Number: 260.3027
Publication Number: 260.3027

Noah Hillman, MD (he/him/his)
Professor
Saint Louis University School of Medicine
St. Louis, Missouri, United States
Presenting Author(s)
Background: Continuous positive airway pressure (CPAP) should be attempted in all spontaneous breathing preterm infants because it decreases rates of bronchopulmonary dysplasia. The type of CPAP nasal interface used affects the pressure transmitted to the nasopharynx and may attenuate the effects of bubble CPAP (BCPAP) on pressure differentials.
Objective: To determine the effects of CPAP nasal prong interfaces and pressures on oxygenation and ventilation during the first 72 hours of life.
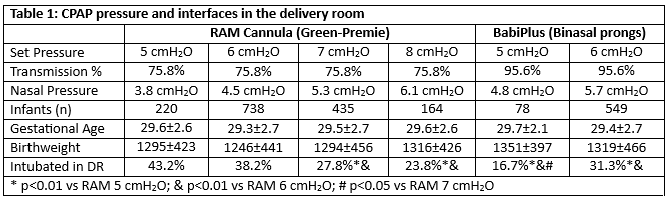
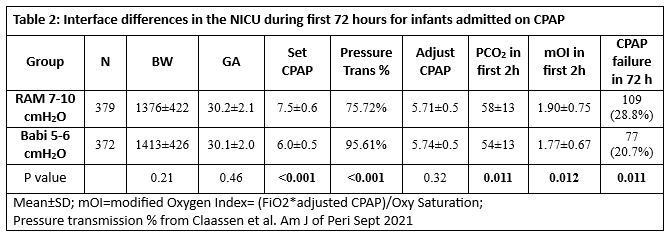
Design/Methods: Data was extracted on all infants born at SSM Health St. Mary’s Hospital between January 2013 and December 2022 with gestational age < 32 weeks and > 500 grams. Electronic query with Microsoft SQL from EPIC extracted respiratory support, oxygenation variables, ventilation variables, vital signs, and respiratory labs for each two-hour period for the first 72 hours of life. SQL code was confirmed by selective chart review. After stabilization with NRP, infants are trialed on BCPAP in deliver room, and based on FiO2 and work of breathing are intubated for prophylactic surfactant in delivery room (DR). Infants were assigned to a DR CPAP interface group (RAM cannula or BabiPlus Nasal prong – short binasal prongs) and pressure based on DOB, or the initial CPAP nasal interface and set pressure on bubble CPAP upon entry into NICU. The transmitted CPAP pressure to nasopharynx was based on previously reported percentages. CPAP failure was use of invasive or non-invasive MV.
Results: Increasing set CPAP pressure (Table 1) decreased intubation in the delivery room, with RAM cannula at 5 to 6 cmH2O having higher failure rate than RAM 7 or 8 cmH2O or BabiPlus 5 or 6 cmH2O. At similar transmitted pressures (Table 2), BabiPlus had decreased PCO2 levels and decreased FiO2 requirements for similar pressures and saturations (modified OI) during the first 4 hours. Less infants failed CPAP in NICU within the first 72 hours in BabiPlus group. When DR and NICU CPAP failure rates are combined, Babi5-6 (42%) and RAM7-10 (45%) were similar but lower than RAM 5-6 (56%) (p < 0.05). There were no differences in respiratory rate, heart rate, mean arterial pressure, apnea events in the first 24 hours, or BPD rates between similar transmitted pressures.
Conclusion(s): Increasing the pressure setting for CPAP decreased intubation rate in delivery room, with comparable rates between interfaces when pressure at nose is similar. BabiPlus (Binasal prongs) have small improvements in ventilation and oxygenation compared with RAM cannula at similar transmitted pressures. RAM cannula at 5-6 cmH2O should be avoided due to suboptimal transmitted pressures.