Developmental and Behavioral Pediatrics
Session: Developmental and Behavioral Pediatrics 5: ADHD and Learning
610 - COVID-19 School Shutdowns and Utilization of School-Based Health Centers: Implications for Supporting Students’ Mental and Behavioral Health
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 610
Publication Number: 610.1995
Publication Number: 610.1995
Connie Cai, AB (she/her/hers)
Student
Johns Hopkins University School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
Background: School-based health centers (SBHCs) integrate health services, including mental health care, into schools, either directly or through comprehensive primary care. The COVID-19 pandemic disrupted students’ mental health as well as access to SBHCs, with impacts still unknown.
Objective: To evaluate and explore K-8 students’ mental and behavioral health and their SBHC utilization before and after COVID-19 school shutdowns.
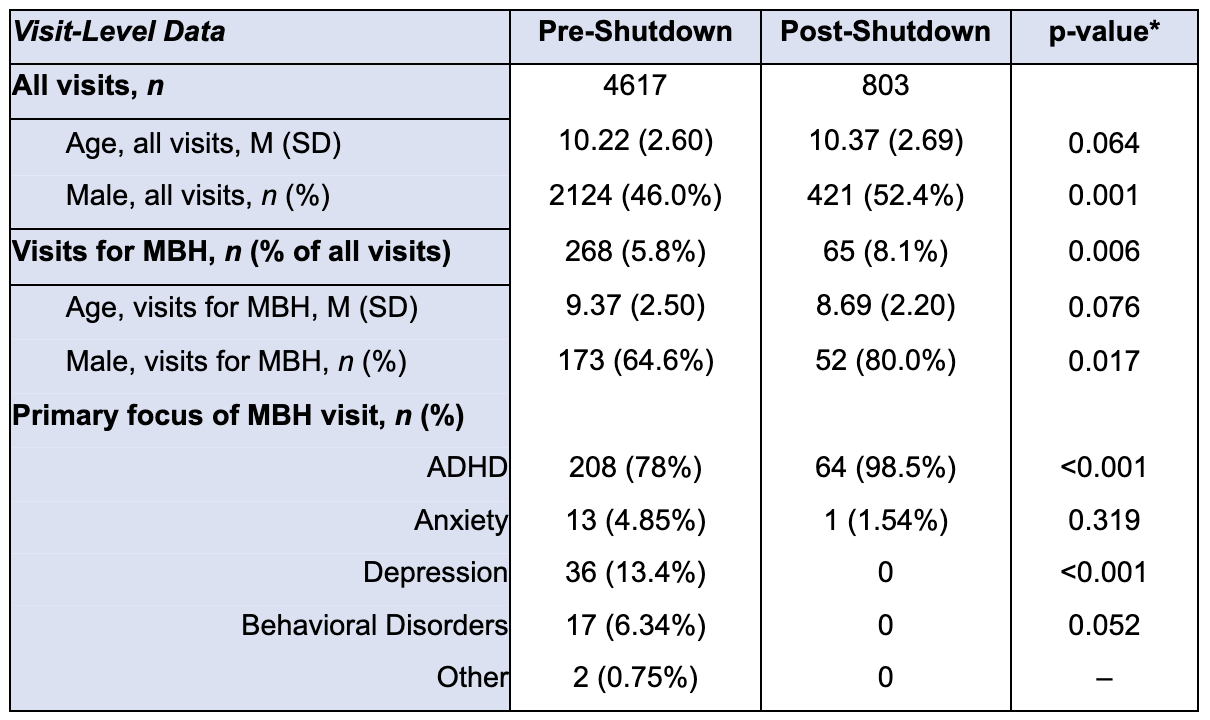
Design/Methods: We used data from the electronic health record (EHR) of a comprehensive SBHC that serves 1600 K-8 students across two co-located Title 1 schools. We compared the proportion of SBHC visits among students with a mental and/or behavioral health diagnosis (MBHD) before (Aug 2016-Mar 2020) and after (Jul 2020-Jun 2022) shutdowns. We further characterized these visits by age, gender, and ICD-10 codes. Incident rate ratios (IRRs) comparing SBHC visit rates among students with and without a MBHD were estimated pre- and post-shutdown (Aug 2018-Mar 2020; Aug 2020-Mar 2022) using multivariable negative binomial regression, controlling for age and gender. To further explore the impact of shutdowns on students’ mental and behavioral health (MBH), we conducted 9 semi-structured, qualitative interviews with teachers (n=3), school administrators (n=2) and SBHC staff (n=4). Interviews were transcribed and coded by two independent coders and emergent themes were identified using NVivo.
Results: The proportion of total SBHC visits (n=5420) by students with a MBHD increased after shutdowns from 11.2% to 13.7% (p=0.04). There was also a significant increase in the proportion of visits with a primary focus on MBH (Table 1). Visits related to ADHD accounted for 78% of visits for MBH pre-shutdown and 98% of post-shutdown visits (p < 0.001). Pre-shutdowns, students with a MBHD were more likely to visit the SBHC compared to students without (IRR 2.18, 95% CI: 1.42-3.35). Post-shutdown, students with a MBHD were more likely to have a SBHC visit, but this difference was not statistically significant (IRR 1.24, 95% CI: 0.72-2.16). All interview informants observed changes in students’ MBH needs, particularly a decrease in students’ attention and behavioral regulation. Teachers reported more interactions with the SBHC and being overwhelmed by students’ needs post-shutdown.
Conclusion(s): Quantitative and qualitative analysis revealed a significant potential impact of school shutdowns, particularly for students with pre-existing MBHDs such as ADHD. Additional support for staff is needed to address students' MBH needs, which may include socio-emotional learning curricula and expanded SBHC partnerships.