Neonatology
Session: Neonatal General 8: ROP, Neurology
307 - Impact of Glycemic Variability on Treatment Requiring Retinopathy of Prematurity
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 307
Publication Number: 307.3050
Publication Number: 307.3050

Radhika Maddali, MD (she/her/hers)
Neonatology fellow
Montefiore Medical Center
Flushing, New York, United States
Presenting Author(s)
Background: Retinopathy of prematurity (ROP) is a vision-threatening disease associated with abnormal retinal vascular development affecting very low birth weight infants; current screening recommendations include neonates with a birth weight (BW) ≤ 1500g or gestational age (GA) ≤30 weeks.
Several studies have been published on ROP and glucose abnormalities; however, the findings have been inconsistent. Hyperglycemia tends to be associated with increased risk of ROP, while the role of glycemic variability (GV) and hypoglycemia has not been established.
Objective: To determine whether ROP requiring treatment is associated with greater variability in concentrations of glucose over the first month of life.
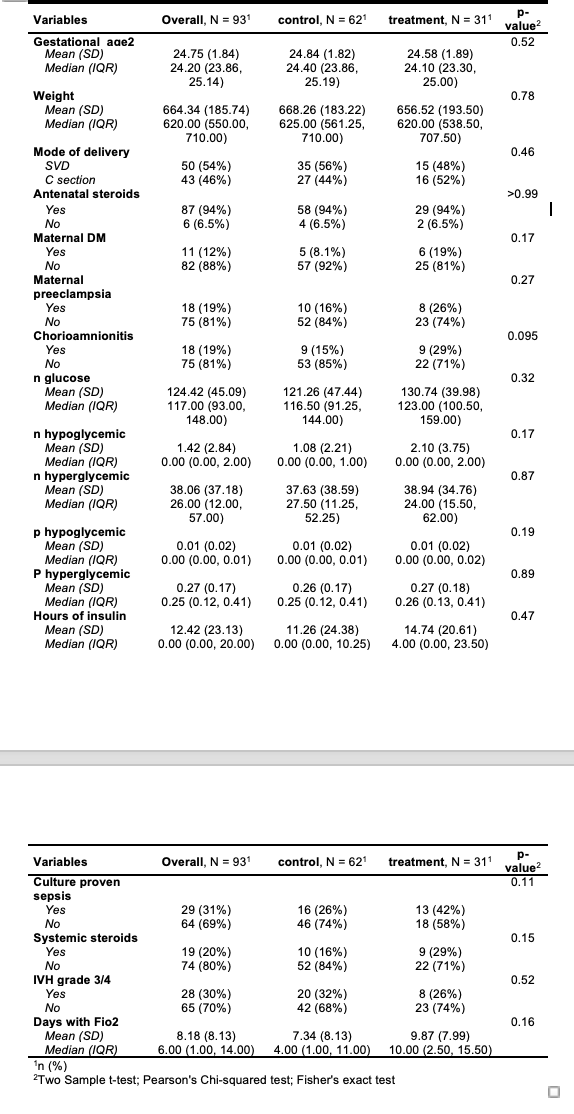
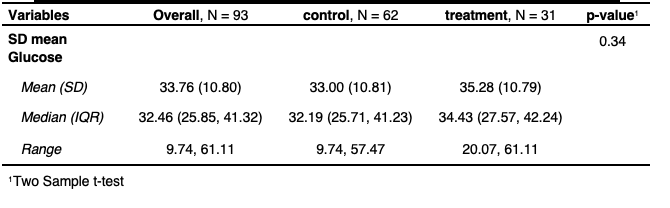
Design/Methods: This is a case-control study of neonates with BW ≤ 1500 gm or GA ≤ 30 weeks evaluated at Montefiore Neonatal Intensive Care Unit from 2017 to 2023 for ROP. Neonates with ROP requiring treatment with laser or bevacizumab were matched for BW and GA with controls with no or less severe ROP in 1:2 case-control ratio. Hypoglycemia was defined as glucose concentration < 45 mg/dl, hyperglycemia as glucose >150 mg/dl, GV was calculated as a standard deviation from the mean glucose concentration for each subject from day 1 to day 28 as well as number of hypo and hyperglycemic episodes. Serum glucose concentrations were obtained using a point-of-care bedside device. Baseline demographic characteristics and clinical outcome variables were compared between the two groups using the two-sample t-test for continuous variables and chi-squared or Fisher’s exact test for categorical variables.
Results: 93 neonates were included for analyses of which 31 had ROP requiring treatment.
There were no significant differences between the baseline demographic data and clinical variables (Table 1). Mean glucose concentration was 130.74 (±39.98) mg/dl in treatment group and 121.26 (±47.44) in control group, p=0.32, with similar rates of insulin administration (p=0.47). The treatment group had higher number of hypoglycemic (2.1 ± 3.75 vs 1.08 ± 2.21, p=0.17) and hyperglycemic episodes (38.94 ± 34.76 vs 37.63 ± 38.59, p=0.87), not statistically significant. The GV is slightly higher in the treatment group (SD=35.28) compared to control group (SD=33.0), but this difference was not statistically significant (p=0.34, Table 2).
Conclusion(s): Our study did not find an association between GV and the development of severe ROP requiring treatment; future research to investigate how GV affects the development of ROP will require multicenter data analysis.