Neonatology
Session: Neonatal General 2: NICU Care Strategies
67 - Consensus Blood Product Transfusion Guidelines for a Large Neonatal Network
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 67
Publication Number: 67.12
Publication Number: 67.12

Lindsay E. Gilmore, MD (she/her/hers)
Neonatal-Perinatal Fellow
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Many neonates and infants hospitalized in the neonatal intensive care unit (NICU) require blood product transfusions, but clinical practices vary widely. Achieving consistency of care across large neonatal networks is very difficult. Emerging evidence has shown that some transfusion practices are harmful for certain NICU patients. Most blood product transfusions are in response to blood count values, as opposed to therapeutic transfusions in the context of active bleeding. This presented an opportunity to ensure consistent evidence-based practices.
Objective: We aimed to establish optimal transfusion guidelines for our 19 hospital neonatal network, through a rigorous 6 month pre-established consensus process including evidence review and expert opinion.
Design/Methods: We reviewed available literature on red blood cell (RBC), platelet, and plasma transfusions, as well as transfusion associated necrotizing enterocolitis (TA-NEC) in the neonatal population. Using a modified Delphi method, we formed consensus guidelines. Ten months after implementation, we surveyed our network to assess guideline utilization.
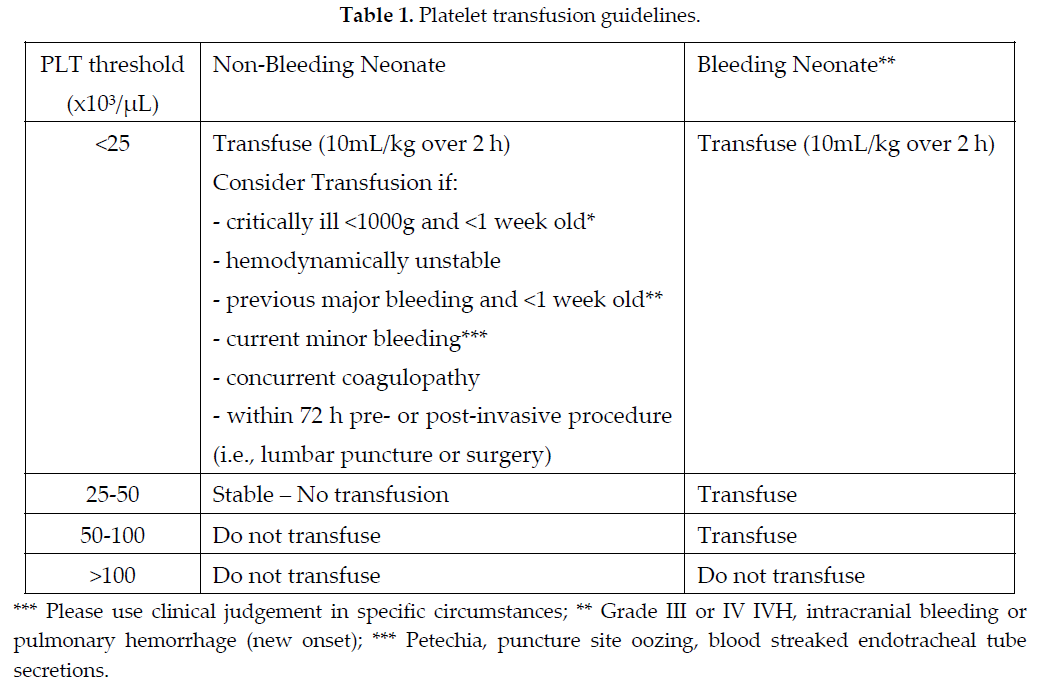
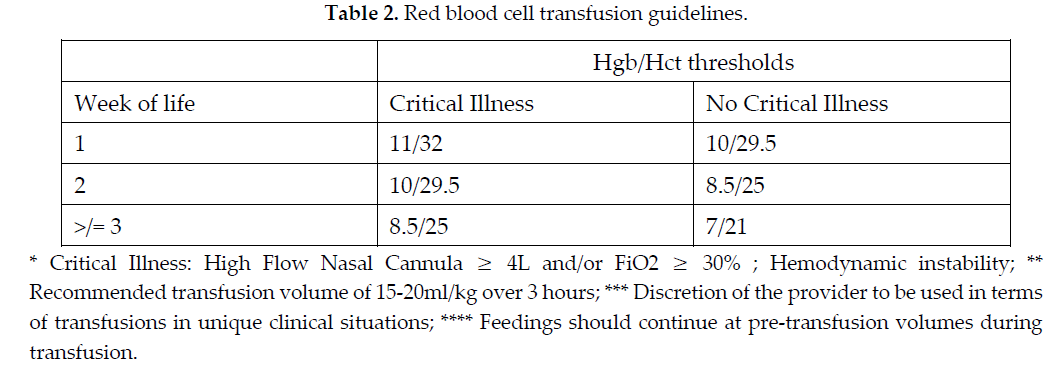
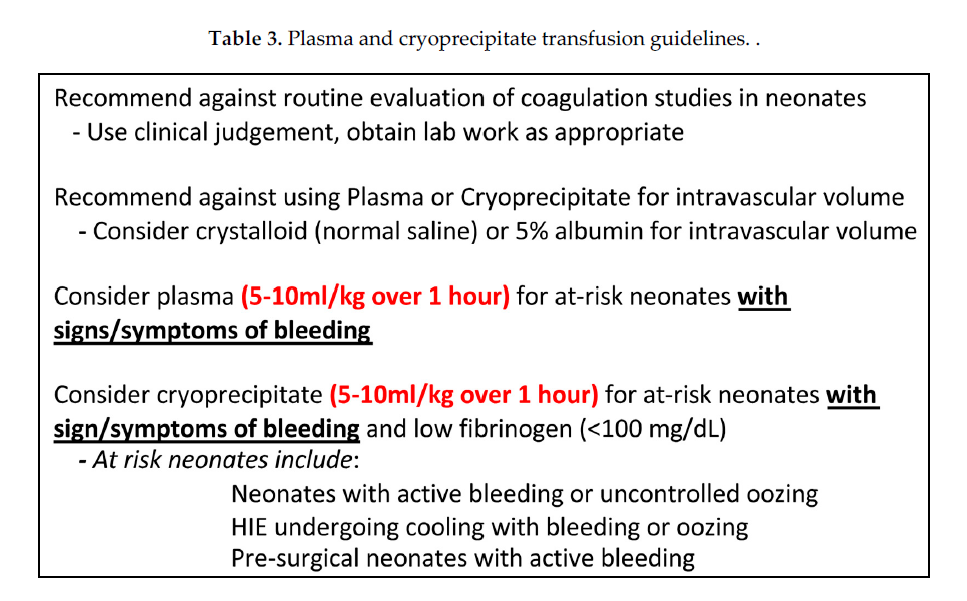
Results: We initially surveyed our neonatal network providers to assess current transfusion practices. Practices notably varied regarding feeding during red blood cell transfusions. Of 102 survey responses, 28% held feeds during RBC transfusions, despite widespread opinion for a lack of strong evidence supporting this practice (88%). Of individuals who held feeds during RBC transfusions, 76% reported willingness to change practice. We then used this data and available literature to develop evidence-based transfusion criteria (Tables 1-3). Given the lack of strong evidence supporting TA-NEC, our guidelines recommend continuing feeds at pre-transfusion volumes during and after RBC transfusions to optimize nutrition. After 6 months, a survey (72 responses) found that respondents (88%) were aware of guidelines and were trying to follow them. After implementation of the guidelines only 6% of respondents held feeds during transfusions without noting a significant change in total NEC rates. Notable practice changes were lowering RBC and platelet transfusion thresholds, giving platelets over 2 hours, limiting platelet transfusions to 10mL/kg, and continuing feeds during RBC transfusions.
Conclusion(s): Neonates and infants are vulnerable patients and emerging studies have shown harm associated with some current blood product transfusion practices. We developed literature-based transfusion guidelines and successfully implemented these across our neonatal care network to improve transfusion practice and safety.