Neonatology
Session: Neonatal Pulmonology - Clinical Science 4: Clinical Practice Questions, Going Home
562 - Tracheomegaly among Extremely Preterm Infants on Prolonged Mechanical Ventilation
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 562
Publication Number: 562.3258
Publication Number: 562.3258

Carlos A. Carmona, Jr., D.O., M.S.
Pediatric ICU Fellow
Children's Hospital of Richmond at VCU
Orlando, Florida, United States
Presenting Author(s)
Background: Positive pressure mechanical ventilation (IPPV) is associated with Bronchopulmonary Dysplasia (BPD) in preterm infants. Airway injuries like subglottic stenosis, tracheomegaly and tracheo-bronchomalacia have also been reported among infants with BPD. It is not clear if the duration of IPPV is associated with the risk of airway injuries
Objective: To determine if prolonged duration of mechanical ventilation (>28 days) in preterm infants is associated with tracheomegaly
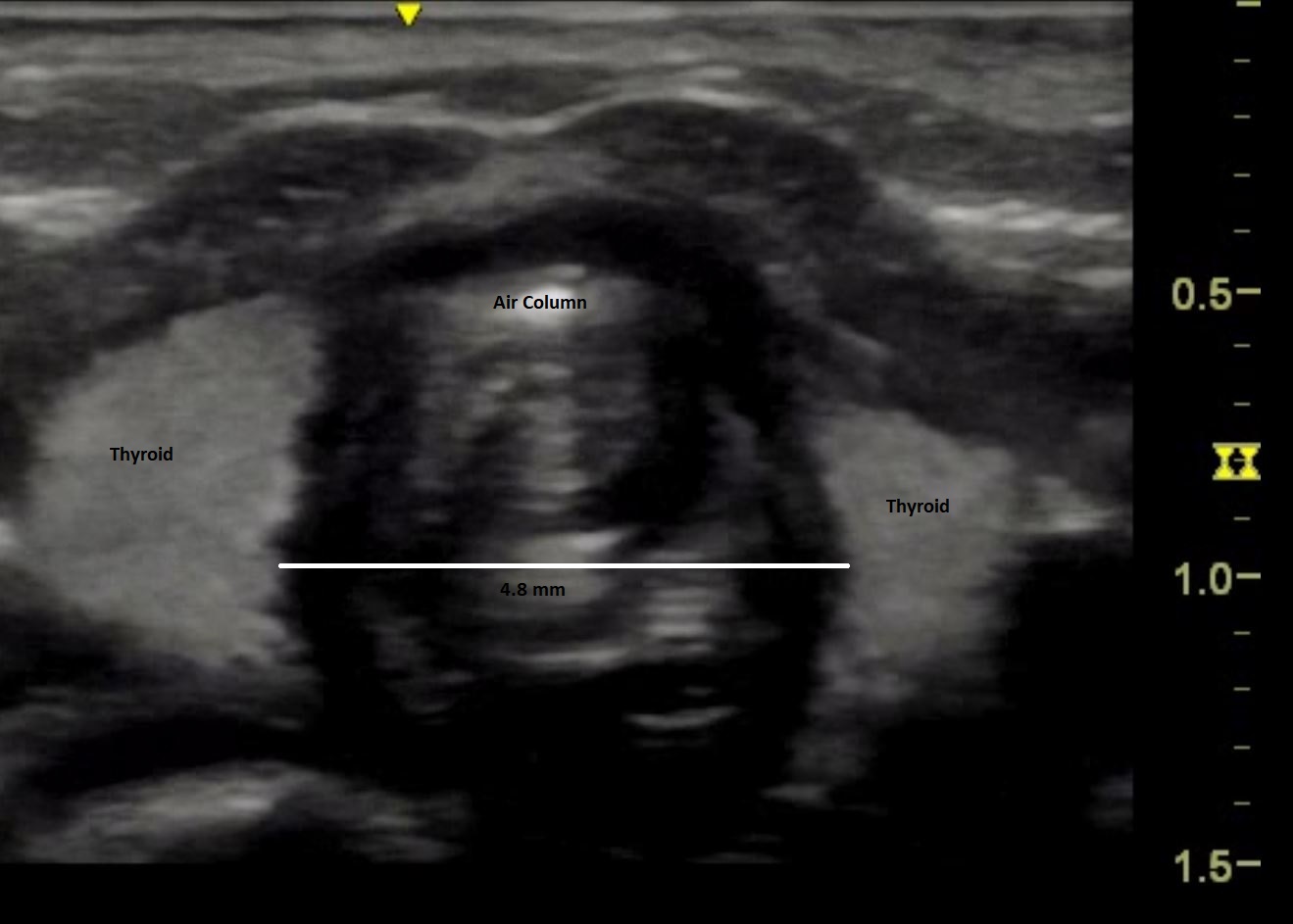
Design/Methods: Extremely preterm infants ( ≤29 weeks) admitted to our Neonatal Intensive Care Unit (Jan 2020- June 2022) were eligible if they required IPPV for ≥ 28 days (prolonged ventilation) or ≤ 7 days (control) in the first 28 days of life. A pediatric sonographer performed tracheal imaging and saved multiple images in short video format. A pediatric radiologist reviewed the imaging and selected 3 different images to measure the tracheal size at sub-glottic level. The average of three measurements was reported as the tracheal size. Following the same protocol, the first 20 scans were also independently reported by another pediatric radiologist. Three measurements by each radiologist were used to determine the intra-observer variability. For inter-observer variability, we used the average tracheal size reported by two radiologists. Body weight on the day of sonography was also recorded. Clinical and demographic data were collected from electronic medical records
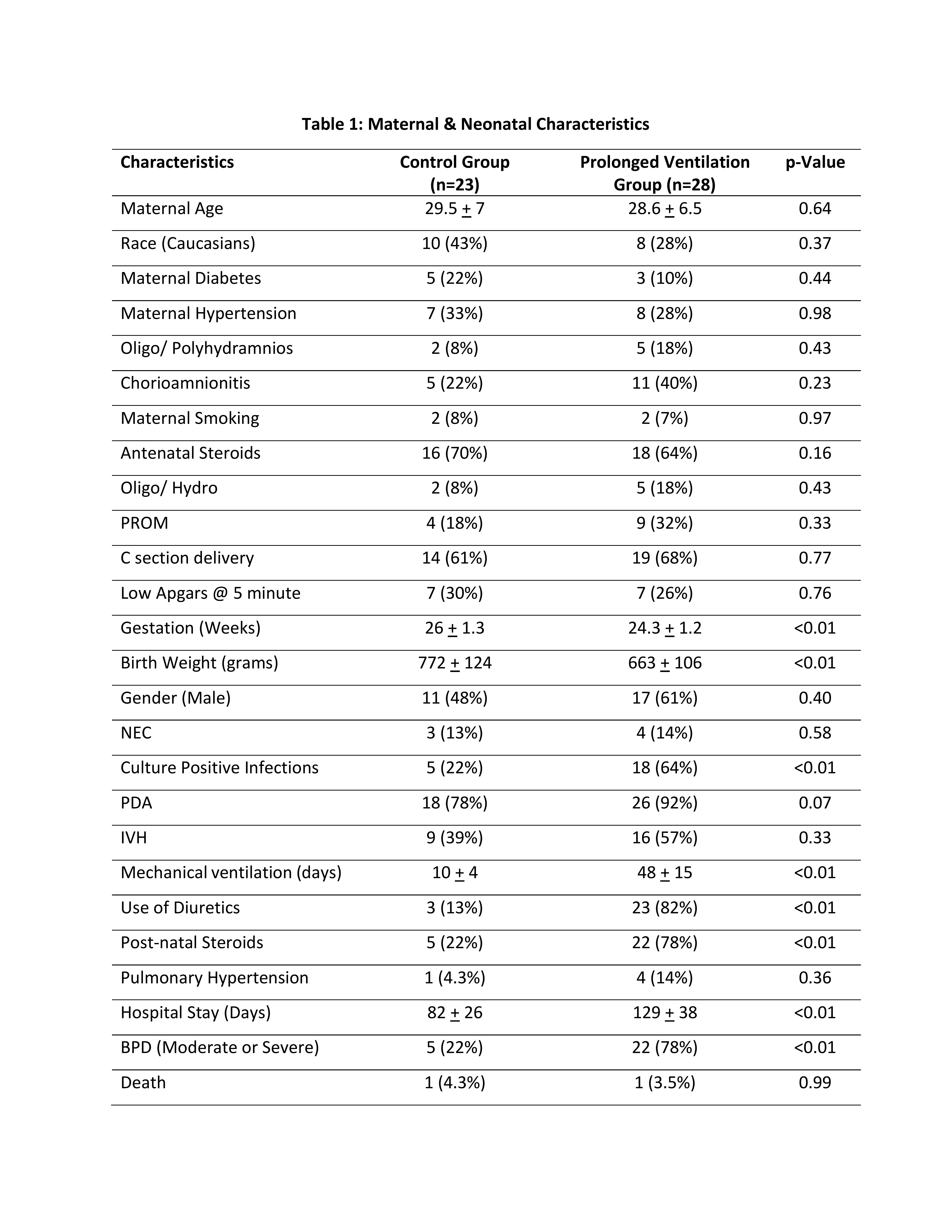
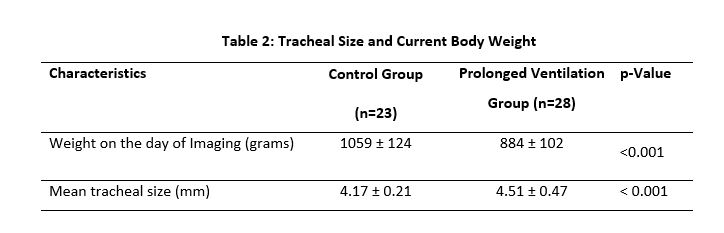
Results: We admitted 417 eligible infants during the study period;80 were excluded as the enrollment was suspended from March to September 2020 due to the COVID-19 pandemic. Eleven infants died prior to 28 days of life, 163 required ventilation for 8 to 27 days of life. Out of the 107 eligible infants, 51 signed our consent for sonography, giving us 23 and 28 infants in the control and prolonged ventilation groups, respectively. Infants in the control group had significantly higher gestation and birth weight. Infants on prolonged mechanical ventilation group were more at risk for infections, BPD and prolonged hospital stay (Table 1). Trachea size was measured as shown in the Figure 1. Inter and intra-observer correlations were 0.83 and 0.97 respectively for a variation of less than 0.05 mm. Infants in the control group had significantly smaller tracheal size (4.17 ± 0.02 vs 4.51 ± 0.04 mm, p < 0.01) despite larger body weight at the time of imaging (1059 + 123 vs 884 +102 grams, p < 0.01). (Table 2).
Conclusion(s): Extremely Preterm infants on prolonged mechanical ventilation (≥ 28days) are at risk for significant tracheomegaly that can be reliably measured by sonography.