Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 1
358 - Now You're Speaking My Language: A Quality Improvement Initiative to Improve the Discharge Process for Spanish-Speaking Patients
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 358
Publication Number: 358.1777
Publication Number: 358.1777

Chloe Kupelian, DO (she/her/hers)
Pediatric Hospital Medicine Fellow
Rady Children's Hospital San Diego
La Mesa, California, United States
Presenting Author(s)
Background: The transition of care from hospital to home is a complex process. Patients with a preferred language of Spanish are more likely to receive inequitable care leading to medication errors, readmissions, and lower patient satisfaction scores. National quality measures advocate for language concordance in verbal and written communication during hospital discharge (DC). We aimed to improve the percentage of Spanish-speaking patients who received translated documents into Spanish prior to DC.
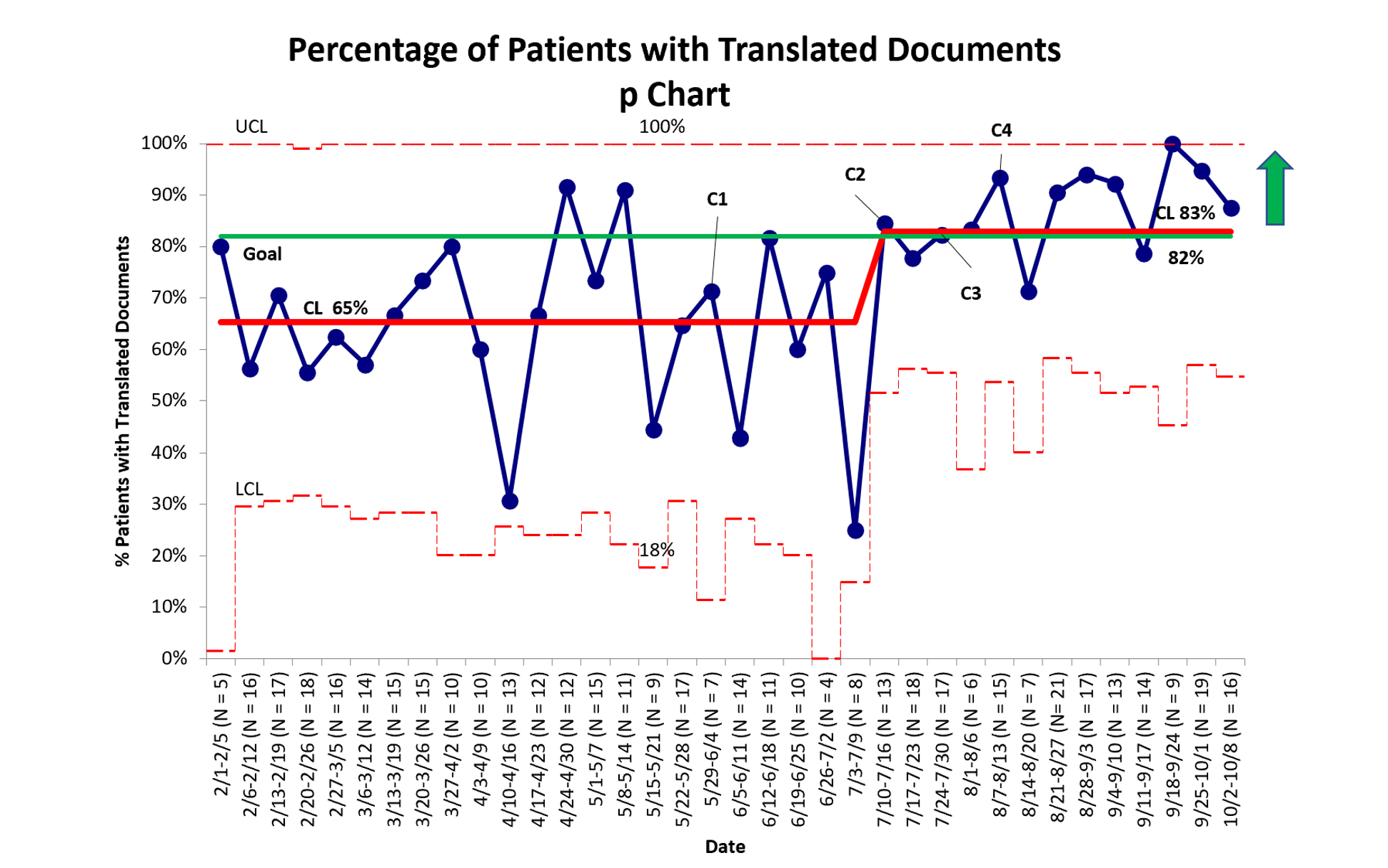
Objective: Our aim was to increase the percentage of Spanish-speaking patients discharged with translated documents from 65% to 82% in 5 months.
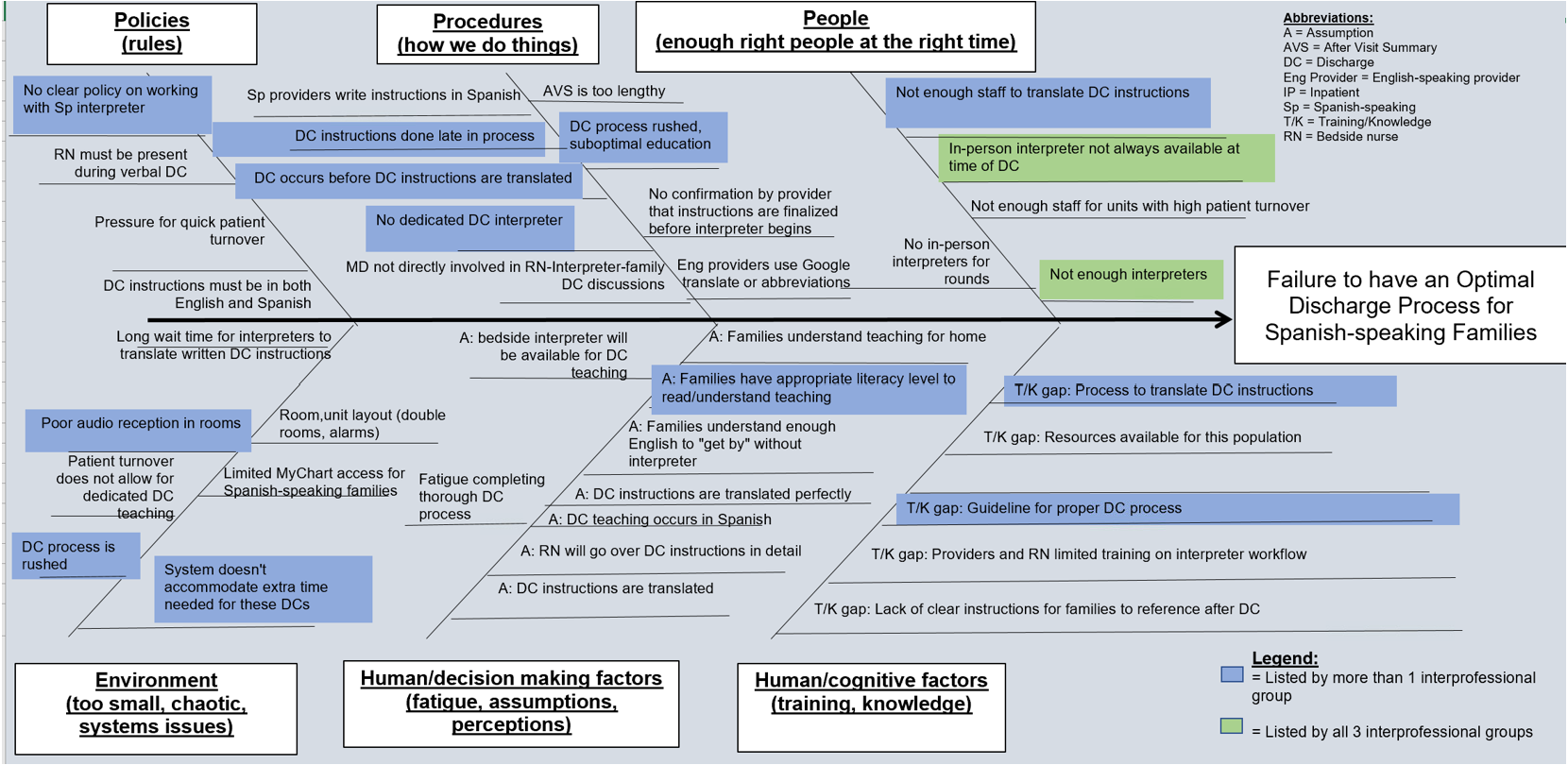
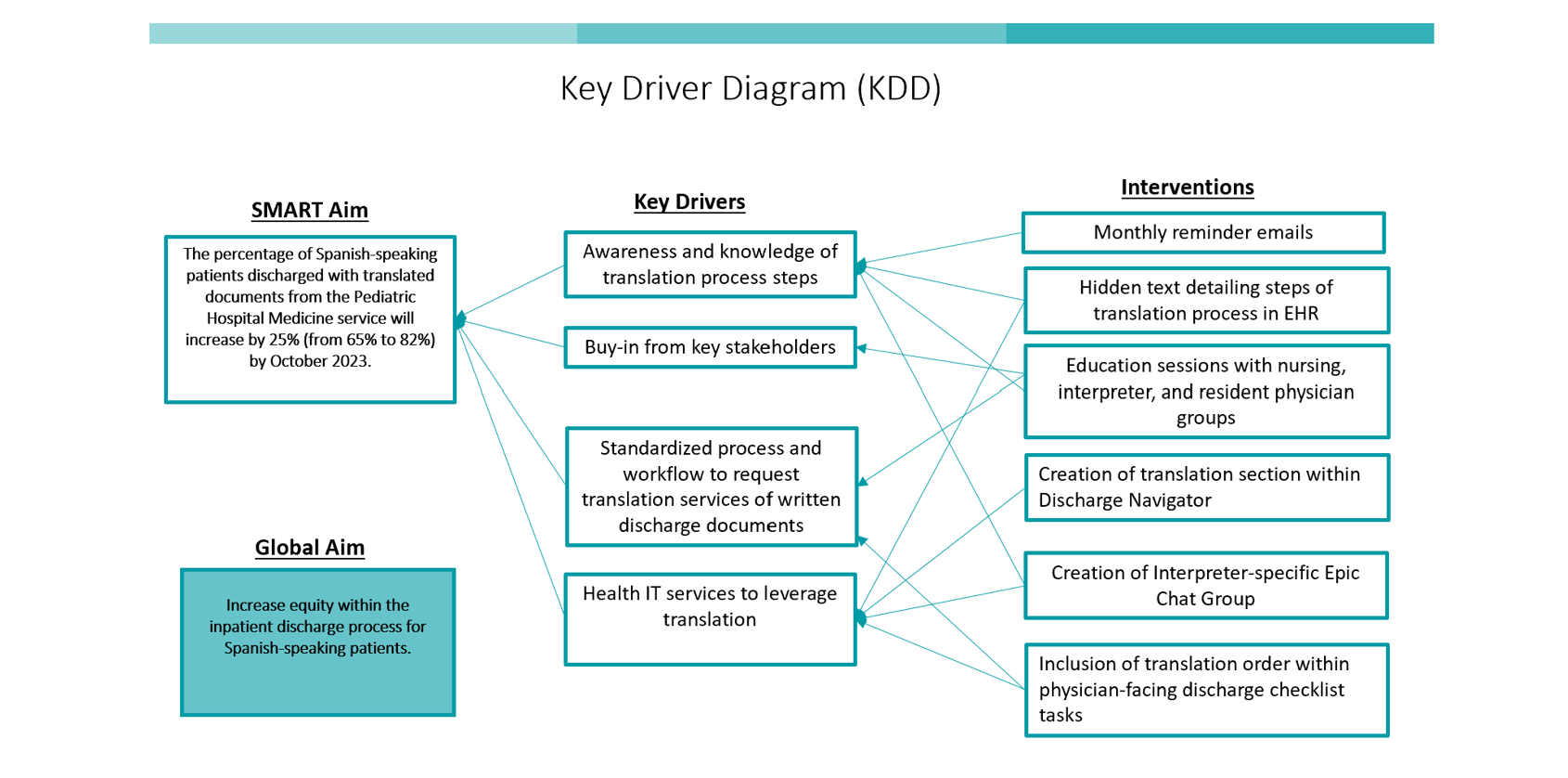
Design/Methods: Plan-Do-Study-Act (PDSA) cycles were conducted. (P): We formed an interdisciplinary team of hospitalists, nurse education leaders, residents, interpreters, and informaticists. We created a process map to highlight each step of a DC. Ishikawa diagrams completed by key stakeholders identified barriers in the process [Figure 1], from this, we created a Key Driver Diagram [Figure 2]. Outcome measure: % of patients with translated DC documents. Balancing measure: length of stay (LOS). Interventions chosen addressed lack of physician education with the translation process and redundant steps identified in the DC process. We prioritized solutions based on feasibility using a prioritization matrix. (D): C1: We modified the physician electronic health record (EHR) DC navigator to include translation order; C2: resident education and training; C3: interpreter and bedside nurse education and training; C4: addition of translation order to DC checklist. (SA): We reviewed data weekly and provided feedback to each group.
Results: Baseline data during February - May 2023 included 225 Spanish-speaking patients discharged from the hospital medicine service; 65% received translated DC instructions. The study period from June - October 2023 included 239 Spanish-speaking patients. We noted special cause variation at the start of Cycle 2 with a centerline shift to 83% [Figure 3]. There was no difference in LOS pre and post interventions (3.23 vs 3.49 days, p = 0.59).
Conclusion(s): Using the Model for Improvement, we achieved our SMART AIM and successfully increased the percentage of Spanish-speaking patients with translated DC documents. The creation of a multidisciplinary team, buy-in from front-line healthcare providers involved in the DC process, and modifying the EHR to streamline and standardize translation workflow were temporally associated with the greatest increases in document translation. Future studies should focus on automaticity within the EHR to increase reliability.