Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 1
432 - Investigating the Efficacy of a Pediatric Social Determinants of Health Screening and Referral Program on Caregiver Anxiety Over Three Months
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 432
Publication Number: 432.179
Publication Number: 432.179
- AW
Annie C. Wolfers, MD (she/her/hers)
Pediatrics Resident Physician
Cohen Children's Medical Center
Forest Hills, New York, United States
Presenting Author(s)
Background: The American Academy of Pediatrics recommends routine screening for Social Determinants of Health (SDOH), as having a high burden of social needs leads to increased emotional distress and anxiety. Many studies have examined the effects of disease on caregiver anxiety, but there are few studies examining the effects of social needs on anxiety, and how those anxiety levels may be alleviated by SDOH screening and referral programs.
Objective: To assess whether providing a patient navigator (PN) to families with unmet social needs decreased caregiver anxiety from baseline to 3-months, compared to providing a resource list alone.
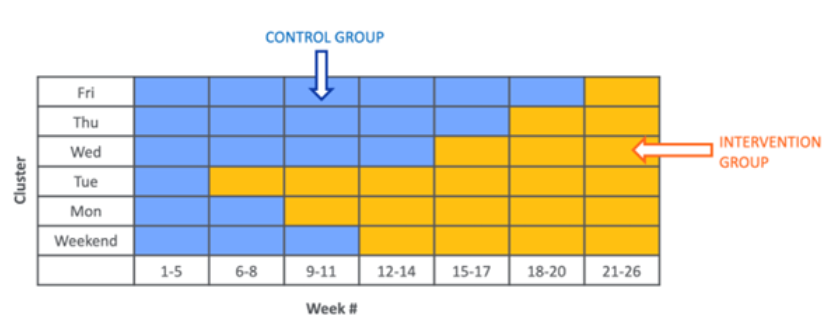
Design/Methods: Between December 2022 and June 2023, we conducted a stepped-wedge cluster randomized trial at a single, large, diverse, academic, pediatric primary care facility. At annual well child checks, families were provided with a list of community resources alone (control), or connected with a PN (intervention) based on the day of the week a patient’s family was seen (Figure 1). The primary outcome was change in anxiety from baseline to 3 months, measured using the 8-item NIH PROMIS-Anxiety Short Form (NPASH), where raw scores can be converted into a T-score with 50 being the average score across the general population. Descriptive statistics were used to understand patient demographic information. An independent t-test was used to determine the effect of the intervention on 3 month follow-up anxiety levels.
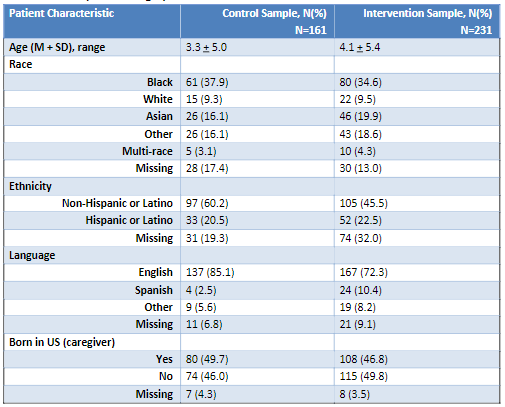
Results: Of the 392 families who completed the NPASH (Table 1), 41.1% (n=161) in the control group, and 58.9% (n=231) in the intervention group screened positive for social needs at baseline. Of those who screened positive for social needs, 29.6% of families (n=115), or 64.6% in the control group (n=75) and 35.3% in the intervention (n=40) completed the baseline and 3-month follow-up. At baseline, mean T-scores in both groups (Table 2) indicate average anxiety as compared to the general population. At three month follow-up, mean T-scores in the control and intervention groups demonstrate slightly greater improvement in anxiety among the participants in the intervention group. However, there was no statistically significant difference in 3 month follow-up anxiety levels between the intervention group (mean change=-.65, SD=10.8) and the control group (mean change=0.8, SD=8.4, p=.420).
Conclusion(s): Providing families who screen positive for social needs with a PN is equally as effective at reducing caregiver anxiety as providing a community resource list alone. This study is limited by a short follow-up period. Further research is needed to assess these findings long-term.
.png)
