Emergency Medicine
Session: Emergency Medicine 8: Mental Health
583 - Demographic, Clinical, and Historical Factors Associated with Medical Admission for Youth Presenting to the Emergency Department for Suicide Attempts by Intentional Self-Poisoning
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 583
Publication Number: 583.1796
Publication Number: 583.1796

Ilana S. Lavina, MD (she/her/hers)
Fellow Physician, Pediatric Emergency Medicine
Children's National Health System
Washington, District of Columbia, United States
Presenting Author(s)
Background: Recent national data indicates that suicide attempts by intentional self-poisoning among youth have been increasing since 2020. This trend mirrors the rising rate of suicidal ideation, attempts, and completions in pediatric patients since the early 2000s.
Objective: To describe recent emergency department (ED) encounters for intentional self-poisoning in youth and to identify demographic, clinical, and historical factors associated with medical admission (as compared to psychiatric admission or discharge), a proxy for morbidity.
Design/Methods: Retrospective cross-sectional study of patients ages 6-17 years who presented to a pediatric tertiary care center with a suicide attempt by self-poisoning between 3/2022 and 2/2023. Encounters with a reason-for-visit or billing code related to ingestion, overdose, or suicide attempt were identified. Accidental or recreational overdoses and suicide attempts by other means were excluded. Demographic, clinical, and psychiatric/social historical data were extracted by manual chart review. Multivariable logistic regression was performed to identify demographic, clinical and historical factors associated with the outcome of medical admission.
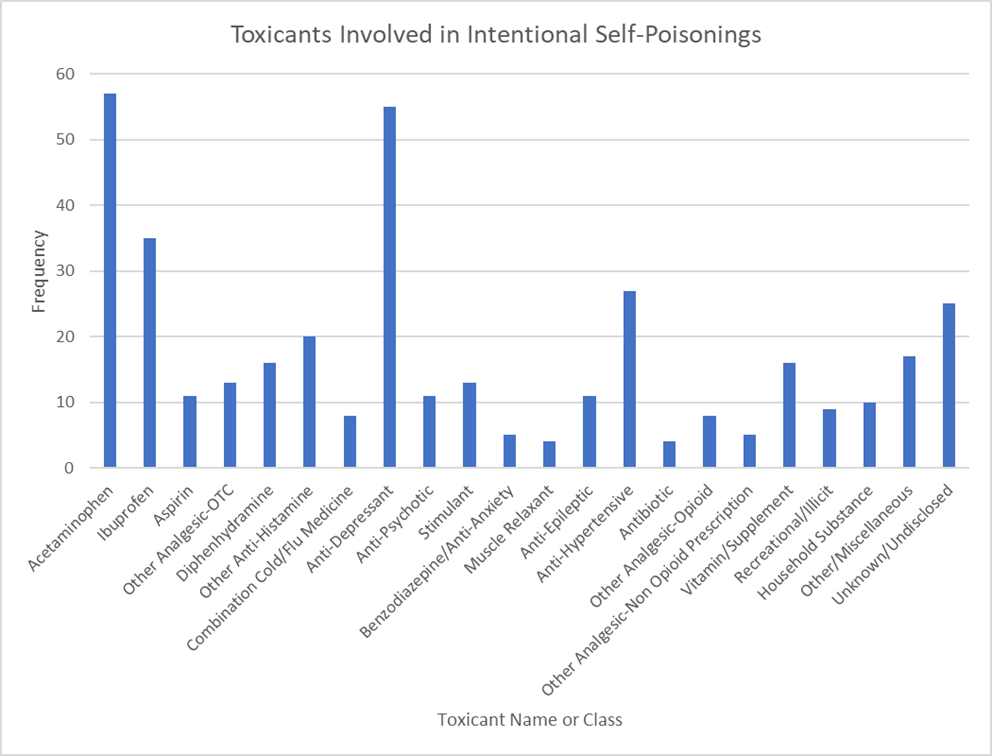
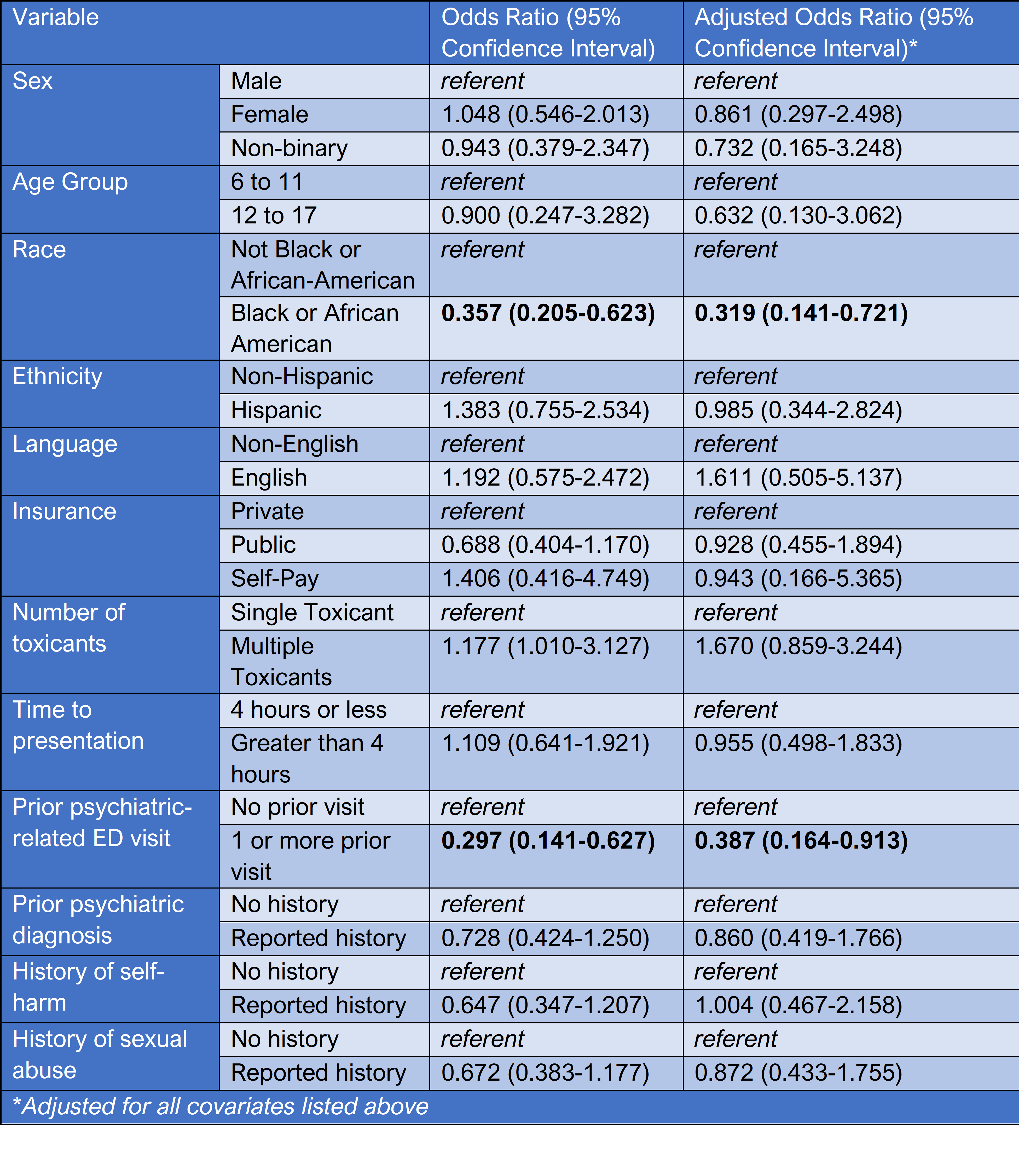
Results: 234 encounters were included. In 64% of encounters, ingestion of a single medication was reported, and in 53%, the patient presented within 4 hours of the ingestion. Acetaminophen and ibuprofen were the most frequent non-prescription toxicants. Antidepressants were the most common prescription toxicant (Fig 1). 62% ingested their own prescribed medication, and 38% ingested a household member’s. 38% required admission to a medical unit or PICU, 47% were admitted to a psychiatric unit, and 15% were discharged from the ED. 69% reported a history of self-harm, 36% reported a history of sexual abuse, and 62% had a prior psychiatric diagnosis. In 23% of encounters, the patient had presented to the ED within the preceding 2 years for a psychiatric concern. Black race and prior psychiatric-related ED visits were associated with lower odds of medical admission (Fig 2).
Conclusion(s): The majority of youth who attempted suicide by self-poisoning used a single medication and presented to ED care promptly. The association between Black race and prior psychiatric-related ED visits and lower odds of medical admission warrants further investigation. Our study adds to the literature by providing detailed insight into the psychiatric and social histories of patients who present with intentional self-poisoning. Future directions include applying our data to inform ED-based interventions such as providing medication lockboxes.