Health Services Research
Session: Health Services Research 1: Workforce
285 - A National Analysis of General Pediatric Inpatient Unit Closures and Openings, 2011-2018
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 285
Publication Number: 285.1473
Publication Number: 285.1473

Carolyn San Soucie (she/her/hers)
PhD Candidate
Harvard University / Boston Children's Hospital
Jamaica Plain, Massachusetts, United States
Presenting Author(s)
Background: Understanding the dynamics of general pediatric inpatient (GPI) unit closures and openings is a key step in assessing the adequacy of hospital-based services for children.
Objective: This paper provides a national examination of: (1) the frequency at which GPI units close or open (with net rates of change); (2) how often closures or openings are due to GPI unit changes only or due to hospital-level changes; and (3) the relationship between hospital financial status or system ownership and GPI unit closures or openings.
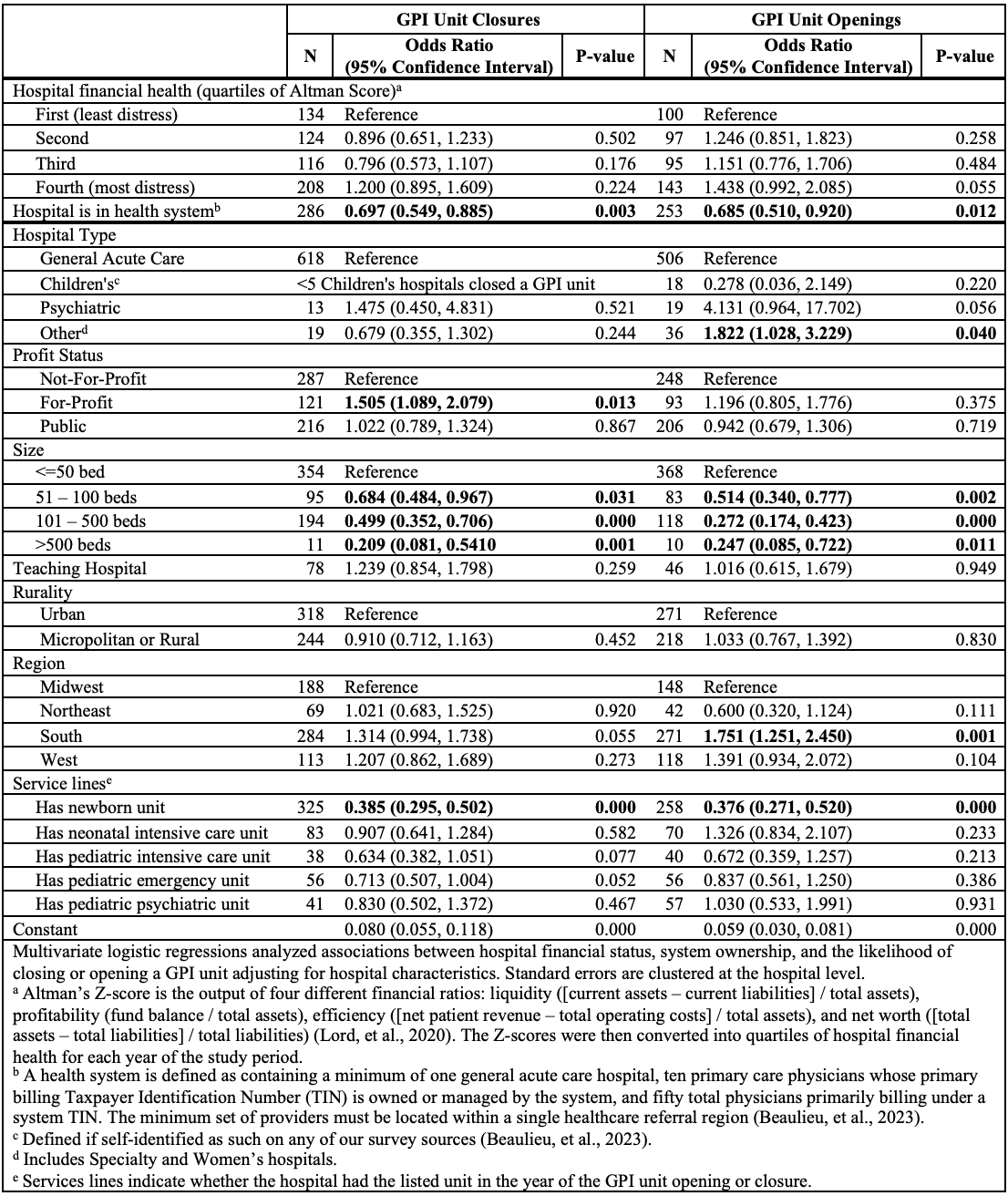
Design/Methods: This descriptive study uses the Health Systems and Providers Database (2011-2018) plus three independent sources of data on hospital closures. We enumerated all GPI unit closures and openings to calculate net rates of change. GPI unit closures were considered to be due to an entire hospital closing if the hospital closure was documented in any one of the three external sources and not if it was not. Because the data is a near-census for the United States, we provide point estimates only. Hospital financial status was characterized by the Altman Z-score, a measure of hospital bankruptcy risk; hospital system ownership was determined by whether the hospital is owned by a larger healthcare organization. Multivariate logistic regressions analyzed associations between hospital financial status, system ownership, and the likelihood of closing or opening a GPI unit adjusting for hospital characteristics (e.g., hospital size and teaching status).
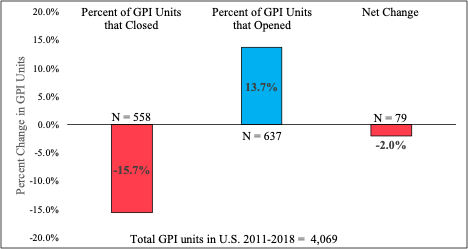
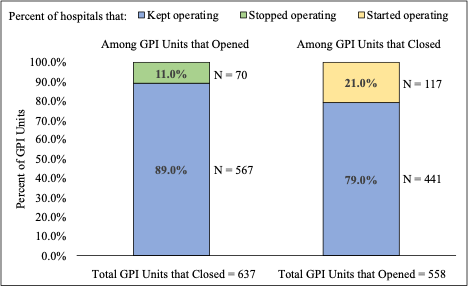
Results: Across the study period, more GPI units closed than opened for a net rate of change of -2.0% (15.7% [637/4,069] closures minus 13.7% [558/4,069] openings). When GPI units closed, 89.0% (567/637) did so in a hospital that otherwise remained open, while 11.0% (70/637) did so when an entire hospital closed. When GPI units opened, 79.0% (441/558) did so in a hospital that was already operating, while 21.0% (117/558) occurred as part of a new hospital. Hospitals with the most financial distress were not any more likely to close a GPI unit (odds ratio: 1.200 [95% confidence interval: 0.895-1.609]) than those with the least, but hospitals owned by systems were significantly less likely to close a GPI unit than hospitals not (odds ratio: 0.697 [95% confidence interval: 0.549-0.885]).
Conclusion(s): Overall, the percentage of GPI units declined between 2011 and 2018, but most frequently involved hospitals that remained operational. Although a hospital’s overall financial status was not associated with GPI unit closures, hospitals belonging to systems were less at risk of GPI unit closures.