Neonatology
Session: Neonatal Pulmonology - Clinical Science 3: Non-Invasive Respiratory Support, RDS
217 - High vs Low CPAP Strategy with Aerosolized Calfactant in Preterm Infants with Respiratory Distress Syndrome
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 217
Publication Number: 217.3148
Publication Number: 217.3148

Dinushan C. Kaluarachchi, MBBS
Associate Professor
University of Wisconsin - Madison
Madison, Wisconsin, United States
Presenting Author(s)
Background: Noninvasive ventilation (NIV) and selective surfactant administration are standard management for respiratory distress syndrome (RDS) in preterm infants. Continuous positive airway pressure (CPAP) is the most commonly used mode of NIV. Use of CPAP is highly variable among neonatal intensive care units. Aerosolized surfactant has been shown to decrease CPAP failure. Optimal CPAP strategy on patients receiving aerosolized surfactant treatment remains unknown.
Objective: To evaluate risk of CPAP failure in preterm infants treated with high vs low CPAP strategy while receiving aerosolized calfactant.
Design/Methods: We performed a secondary analysis of preterm infants with RDS who received aerosolized calfactant under AERO-02 clinical trial and AERO-03 expanded access program. Analysis was restricted to subjects with gestational age (GA) between 29 0/7–36 6/7 weeks and on CPAP. Infants were divided into two groups based on level of CPAP at the initiation of aerosolized calfactant treatment (Low, 4-7; High, 8-10 mm H20). Chi-square and Wilcoxon rank-sum tests were used to make comparisons between groups. Logistic regression model was used to determine the association between demographic characteristics and odds of CPAP failure, which was defined as intubation for liquid surfactant administration or need for mechanical ventilation.
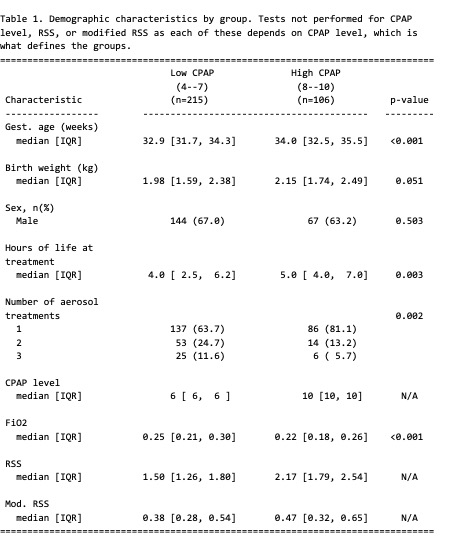
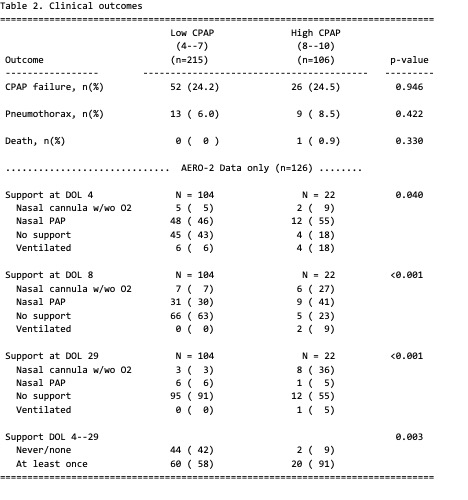
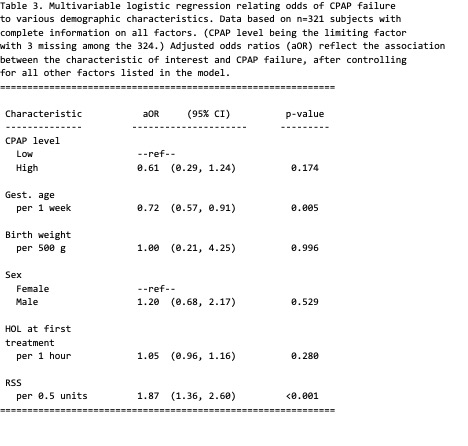
Results: A total of 321 infants were included in the study (215 in the low CPAP group and 106 in the high CPAP group). Those in the high CPAP group tended to be of greater GA, be older at time of first aerosolization, have fewer aerosol treatments overall, and have lower FiO2 levels (Table 1). Clinical outcomes of CPAP failure, pneumothorax and death were not different between the two groups (Table 2). Odds of CPAP failure were not different between the two groups after adjustment of variables (OR = 0.61; 95% CI: 0.29, 1.24) (Table 3). Higher proportion of infants remained on respiratory support in the high CPAP group at day 3, 7 and 28 (data limited to AERO-02 (n=126) (Table 2).
Conclusion(s): We found no difference in CPAP failure among infants who received aerosolized calfactant that were treated with high vs low CPAP strategy. Although data were limited, a high CPAP strategy did lead to significantly longer time on support. Long-term respiratory outcomes of high vs low CPAP strategy in infants treated with aerosolized calfactant needs to be evaluated on large randomized controlled trials.