Neonatology
Session: Neonatal Neurology 6: Clinical
555 - Higher Mortality and Resource Utilization in Term and Preterm Neonates with Seizures Using the HCUP-NIS 2016-2020 National Database
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 555
Publication Number: 555.1495
Publication Number: 555.1495
- EC
Erwin T. Cabacungan, MD, MPH
Associate Professor
Medical College of Wisconsin
MIlwaukee, Wisconsin, United States
Presenting Author(s)
Background: Neonatal seizures are a critical neurological emergency with high morbidity and mortality in the perinatal period. Advances in detection for both term (TermSz) and preterm (PretermSz) neonates with seizures allow for better diagnostic ability and categorization. We hypothesize that TermSz and PretermSz would lead to increased mortality and resource utilization than those without seizures.
Objective: To assess the association between neonatal seizures and underlying risk factors and coexisting morbidities in term and preterm neonates and determine mortality and resource utilization using a recent national database.
Design/Methods: We conducted a retrospective cohort study of in-hospital births for neonates with seizures (ICD-10-CM code P90) using the 2016–2020 Healthcare Cost and Utilization Project National Inpatient Sample (HCUP-NIS). We stratified the cohort for analysis into TermSz and PretermSz and those without. Weighted analyses ensured nationally representative estimates. Logistic regression was used for the outcome death, a generalized linear model with Poisson distribution for length of stay (LOS), and gamma distribution for total charges. Analyses were adjusted for covariates demographics, hospital-level characteristics, antenatal and intrapartum risk factors, and comorbidities.
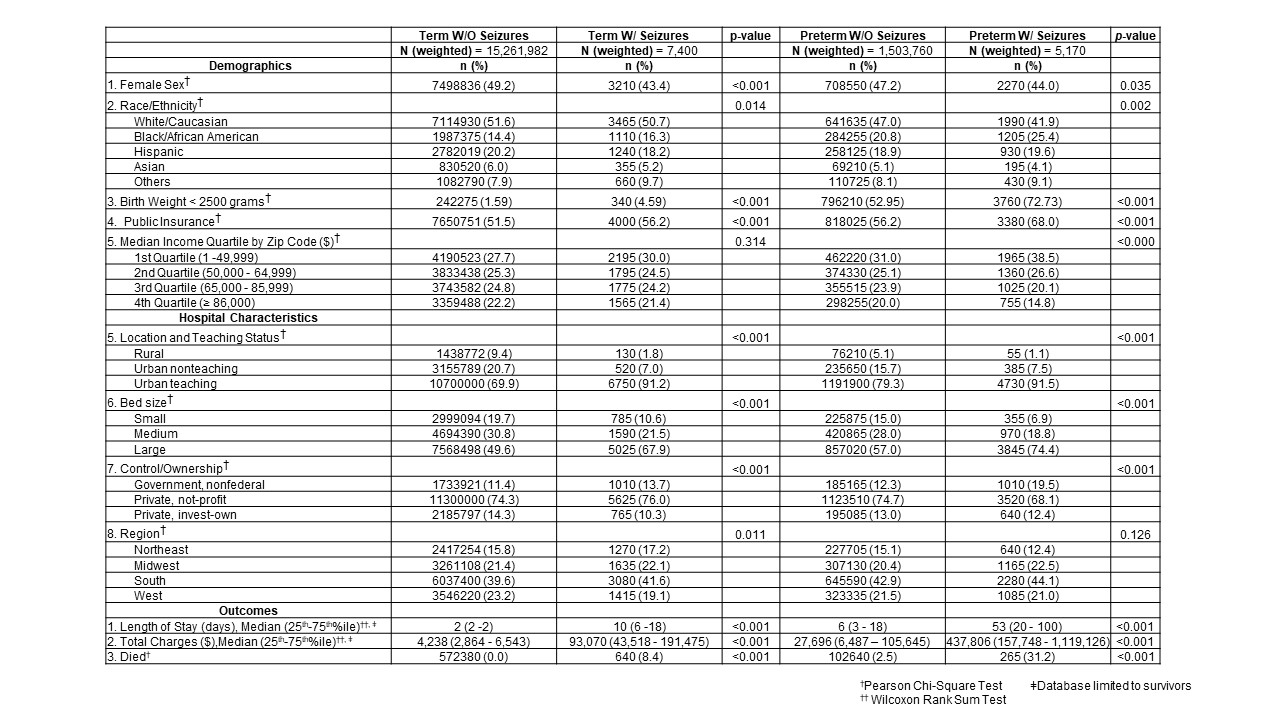
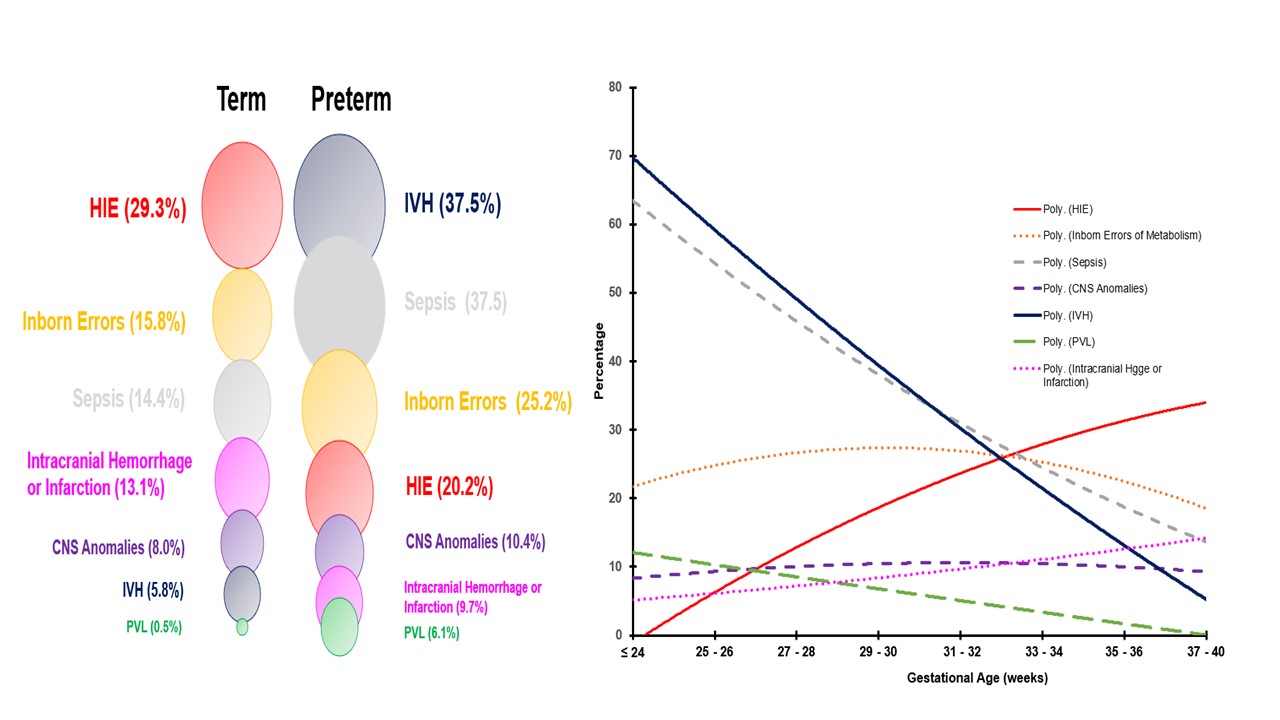
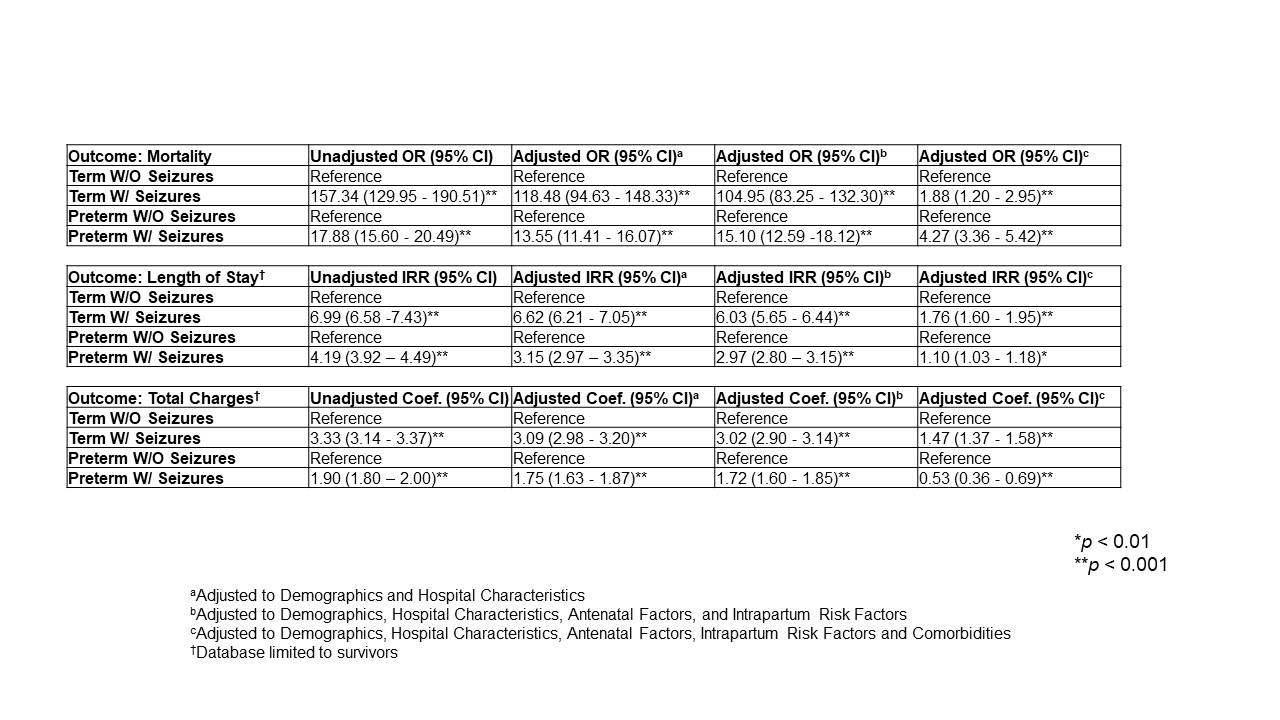
Results: The dataset included 16,778,312 neonates, with 4 per 10,000 (7,400) weighted discharges being TermSz and 3 per 10,000 (5,170) weighted discharges being PretermSz. There were significant differences in TermSz and PretermSz compared to those without seizures in demographics, hospital characteristics, and outcomes (Table 1). Among TermSz vs. PretermSz, we observed a differential prevalence of hypoxic-ischemic-encephalopathy (HIE) (29.3% vs. 20.2%), intracranial hemorrhage and infarction (13.1% vs. 9.7%), sepsis (14.4% vs. 37.5%), and intraventricular hemorrhage (IVH) (5.8% vs. 37.5%), Fig 1A. As gestational age progresses, IVH and sepsis significantly decrease, whereas HIE and intracranial hemorrhage and infarction trend upwards, Fig 1B. Both TermSz and PretermSz demonstrated increased mortality rates (2-fold and 4.3-fold); increased length of stay (1.8-fold and 1.1-fold); and increased total charges for TermSz (1.5-fold) but decreased for PretermSz (0.5-fold) compared to those without seizures (Table 2).
Conclusion(s): This study highlights the evolving prevalence of comorbidities in neonates with seizures as gestational age advances. Despite advances in neonatal care improving outcomes, TermSz and PretermSz have higher mortality and resource utilization in a modern cohort of hospitalized neonates.