Health Services Research
Session: Health Services Research 2: Novel Methods and Disparities
300 - Feasibility, Acceptability, and Appropriateness of Social Risk Screening Implementation in an Inpatient Community Hospital Setting
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 300
Publication Number: 300.1433
Publication Number: 300.1433
- JL
Jana C. Leary, MD, MS (she/her/hers)
Assistant Clinical Professor
Tufts Medical Center
Waban, Massachusetts, United States
Presenting Author(s)
Background: The AAP recommends screening for social risks at all child health visits. A growing number of hospitals are now implementing social risk screening systems, but all pediatric studies to date have been conducted in children’s hospitals.
Objective: We aimed to assess the feasibility, acceptability, and appropriateness of implementing a social risk screening and referral system in a resource constrained community hospital setting.
Design/Methods: In April 2022, a local community hospital in MA implemented a universal pediatric social risk screening and referral system. From March-October 2023, we used a concurrent mixed methods approach to evaluate its implementation. We surveyed clinicians who perform screening (nurses) or respond to screening (social workers, physicians, case managers) and parents of hospitalized children, assessing implementation outcomes–feasibility, acceptability, and appropriateness–using validated measures based on 5-point Likert scales. Mean measure scores ≥ 3 were used to define a positive implementation outcome. We concurrently performed 15 semi-structured interviews with clinicians and parents, linking interview transcripts with the quantitative measures and analyzing interviews thematically.
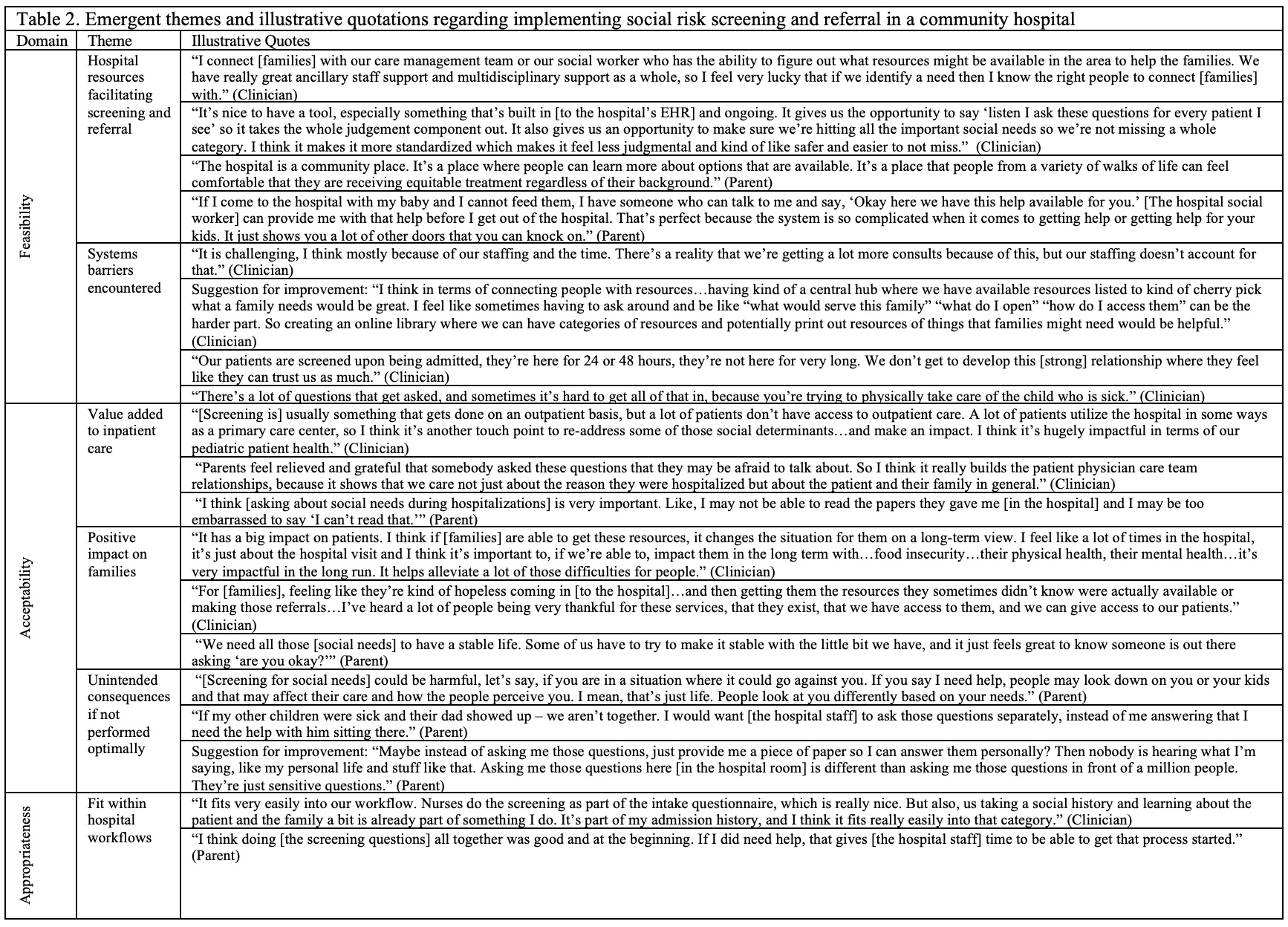
Results: Thirty-one clinicians (78%) and 20 parents (80%) completed surveys. Among clinicians performing screening, 94% rated the social risk screening and referral system as feasible, 89% as acceptable, and 94% as appropriate. Among clinicians responding to screening, 100% rated the system as feasible, acceptable, and appropriate. Among parents, 100% rated the system as feasible and acceptable, and 95% as appropriate (Table 1). Emergent interview themes included value added to inpatient care, positive impact on families, unintended consequences if not performed optimally, hospital resources facilitating screening/referral, systems barriers encountered, and natural fit within hospital workflows (Table 2).
Conclusion(s): Implementation of a pediatric inpatient social risk screening and referral system was feasible, acceptable, and appropriate in a real-world community hospital setting; however, systematic barriers and key areas for improvement were identified. Implementation outcome ratings were relatively lower for clinicians performing screening. Development of standardized education for clinicians regarding social risk screening and response may prove helpful as more institutions implement social care programs. Future directions will include implementation research adapting the screening and referral program based on stakeholder feedback.
.jpg)