Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 3: Pulmonary Hypertension and Prematurity
112 - Does treatment of a PDA in extreme preterm infants affect clinical outcome?
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 112
Publication Number: 112.1943
Publication Number: 112.1943

Markus K. Tauscher, MD (he/him/his)
Neonatologist
Peyton Manning Children's Hospital at St. Vincent
Indianapolis, Indiana, United States
Presenting Author(s)
Background: A PDA associated left-to-right shunt causes increased pulmonary blood flow and ductal steal from the systemic circulation and thus can have adverse effects on extreme premature infants. The benefits of actively treating a PDA are controversial and treatment is associated with acute and possible longterm adverse effects. Therefore, consensus as to when to obtain an echocardiogram and if or how to treat a PDA is difficult to achieve.
Objective: To compare morbidity and mortality of infants born < 29 weeks who were diagnosed and treated for a PDA to infants diagnosed with a PDA but who did not receive treatment.
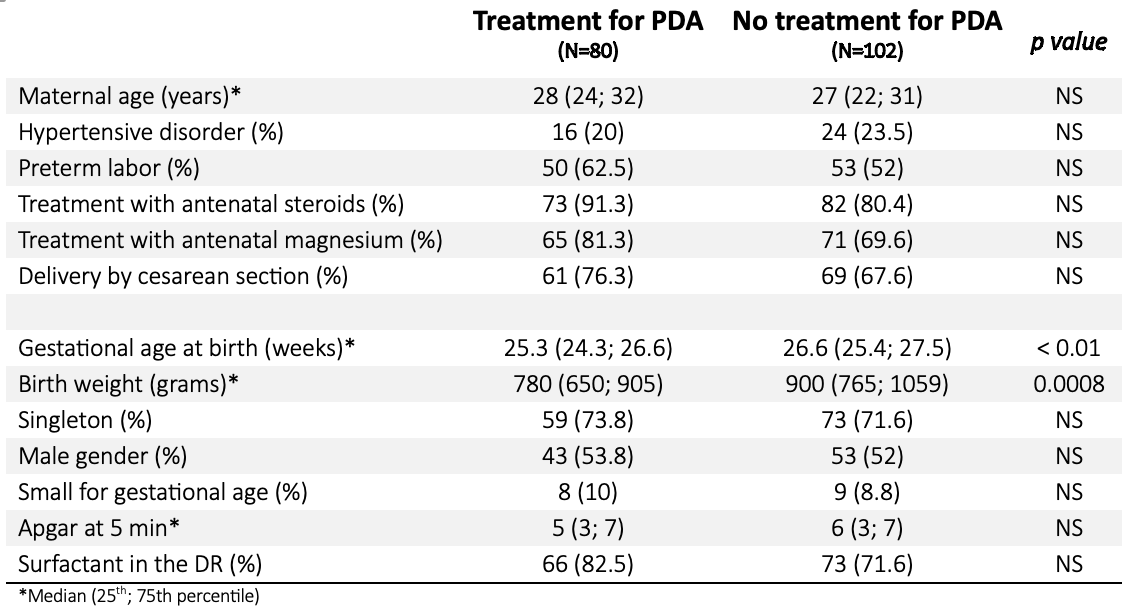
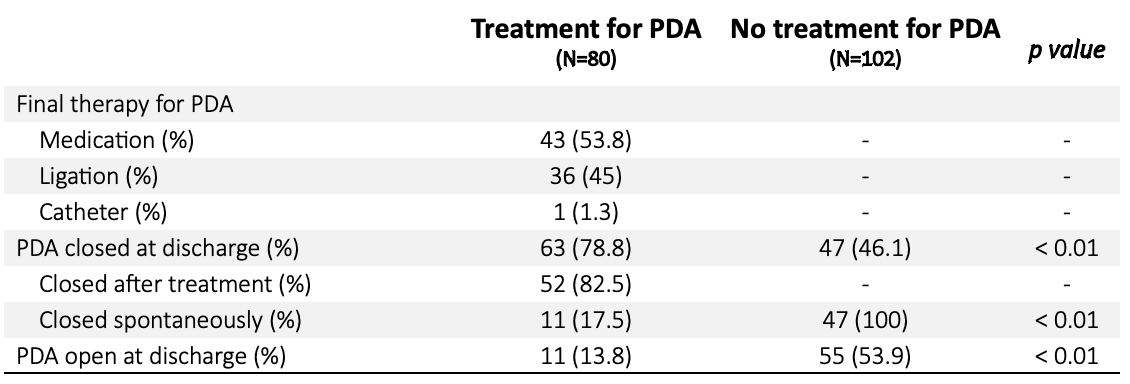
Design/Methods: This is a retrospective cohort study on preterm infants born < 29 weeks gestation at birth, who were admitted to a level IV NICU between 2016 to 2021 and were diagnosed with a PDA by echocardiogram. Infants were divided into 2 groups: infants diagnosed with a PDA who received treatment and infants diagnosed with a PDA and did not receive treatment. Decisions as to when to obtain an echocardiogram and if or how to treat a PDA (COOX inhibitor, acetaminophen, surgical ligation or transcatheter device closure) were at the sole discretion of the clinical team caring for an infant with a PDA. Data including maternal and neonatal characteristics, morbidity and mortality were collected from the electronic medical record and compared between the two groups.
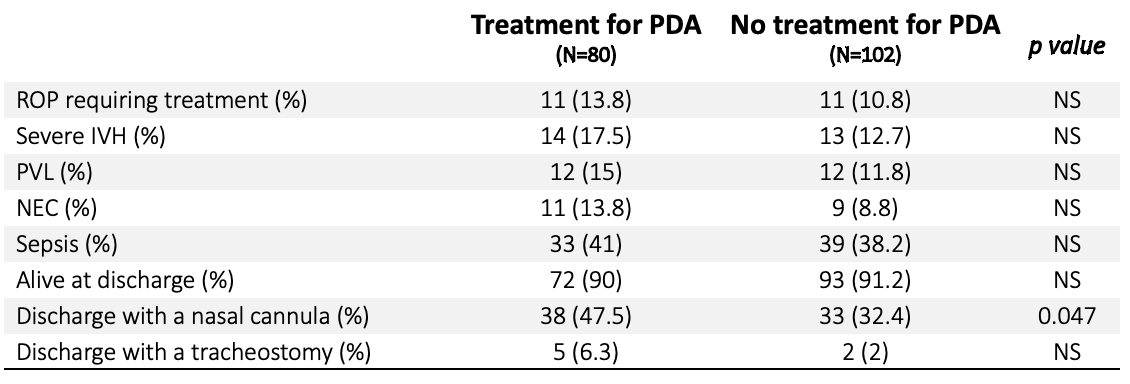
Results: 182 preterm infants < 29 weeks were diagnosed with a PDA by echocardiogram: 96 infants received treatment and 103 did not receive treatment for a PDA. Infants who were treated for a PDA had a lower gestational age (25.3 vs 26.6 weeks, p< 0.01) and birth weight (780 vs 900g, p< 0.01) compared to those who did not receive treatment. Although the PDA closure rate was higher in the treatment group, spontaneous closure occurred in infants who did not receive treatment (78.8 vs 46.1%, p< 0.01). The incidence of severe IVH, ROP requiring treatment, PVL, NEC, sepsis, discharge with a tracheostomy and death was the same in both groups. Only the percentage of infants requiring oxygen at discharge (47.5 vs 32.4%, p< 0.05) was higher in infants who received treatment for a PDA.
Conclusion(s): Our findings suggest that treatment of a PDA did neither improve neonatal morbidity nor mortality, but infants who received treatment had a significantly lower gestational age at birth and a lower birth weight. Younger gestational age and lower birth weight is often associated with higher morbidity and mortality. Therefore, a benefit of treating a PDA cannot be excluded.