Neonatology
Session: Neonatal Neurology 4: Clinical
526 - Preterm Brain Growth is Strongly Correlated with Cumulative Autonomic Stress
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 526
Publication Number: 526.1406
Publication Number: 526.1406
Zachary A. Vesoulis, MD, MSCI
Assistant Professor
Washington University in St. Louis School of Medicine
St. Louis, Missouri, United States
Presenting Author(s)
Background: Preterm infants experience many sources of inflammation and stress in the NICU including sepsis, mechanical ventilation, painful procedures, and hypoxia. Although linked with adverse neurodevelopmental outcomes, no method exists to quantify their continuous or cumulative impact. We previously demonstrated that computational analysis of streaming physiologic data detects inflammatory conditions and therefore may provide a useful basis to quantify inflammatory stress.
Objective: To quantify inflammatory stress through a novel physiologic biomarker and relate cumulative measures to regional brain growth at term-equivalent age (TEA).
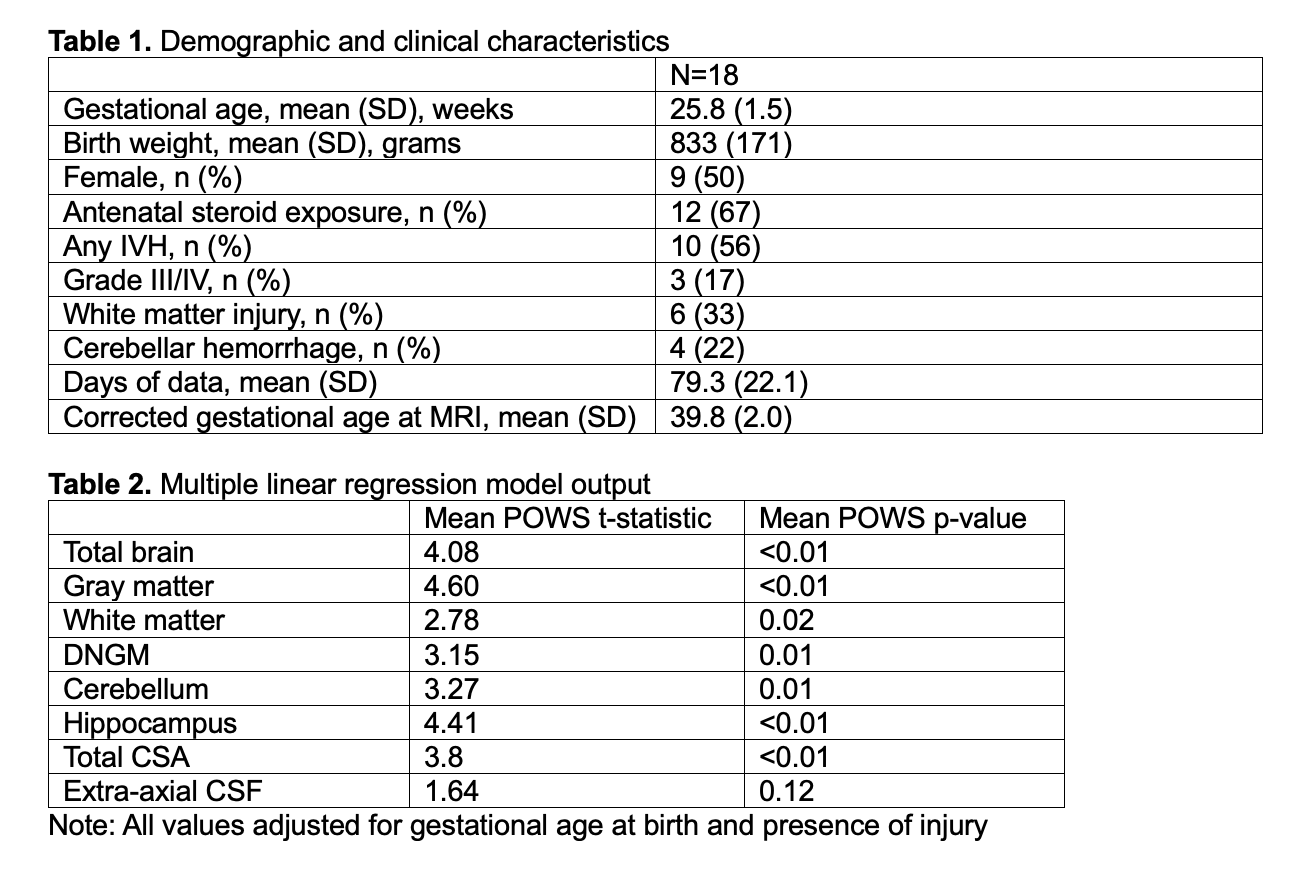
Design/Methods: Infants born < 32 weeks gestational age were prospectively enrolled in a longitudinal physiologic monitoring study with term-equivalent MRI. Heart rate (HR) and pulse oximetry (SpO2) were recorded every 2 sec from admission to discharge. Infants were excluded if they died before MRI or if there was less than 80% vital sign data coverage.
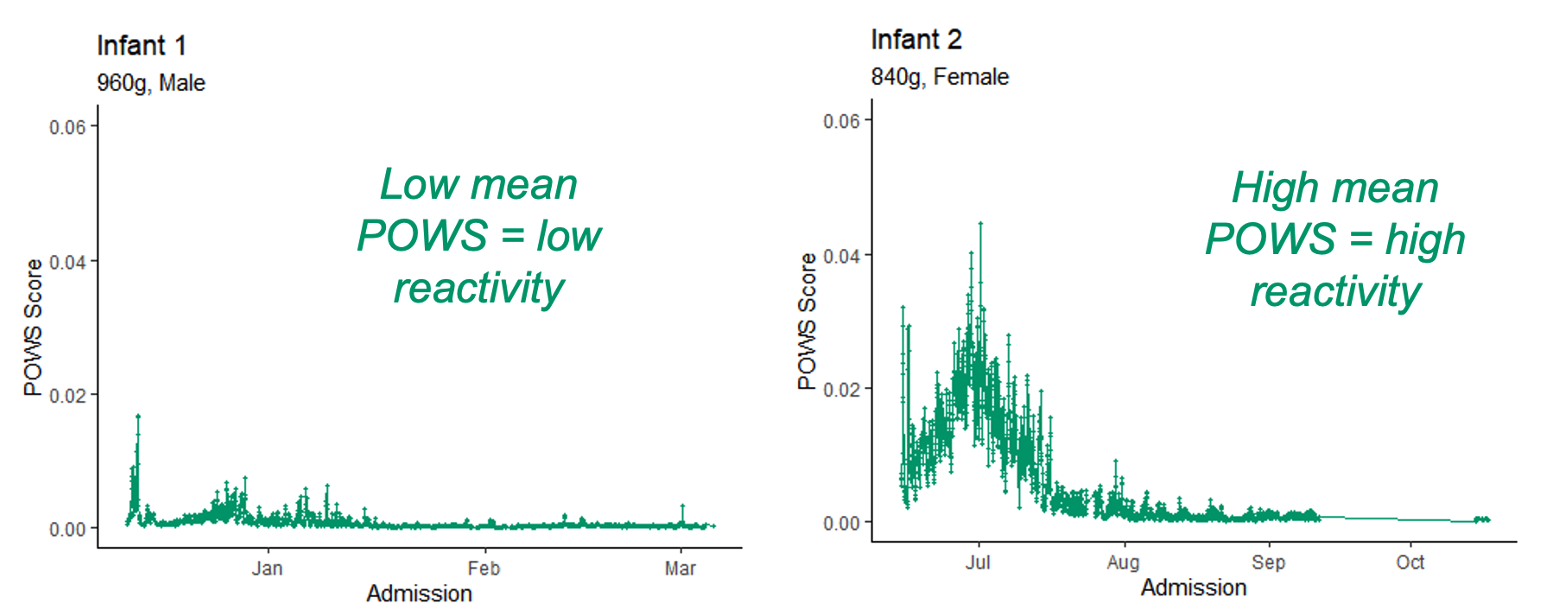
A pulse-ox warning score (POWS) was calculated from the mean, SD, skewness, and kurtosis of HR/SpO2 and their cross correlation. One score was generated for every hour of data and the mean POWS was calculated from all available scores. Examples are shown in Figure 1.
Using the M-CRIB-S pipeline and parcellation scheme, cortical surface extraction, surface registration and atlas-based cortical parcellation was performed from T2 images. Eight brain growth metrics were calculated including total cortical surface area, gray matter, white matter, deep nuclear gray matter, cerebellum, hippocampus, and total brain volume.
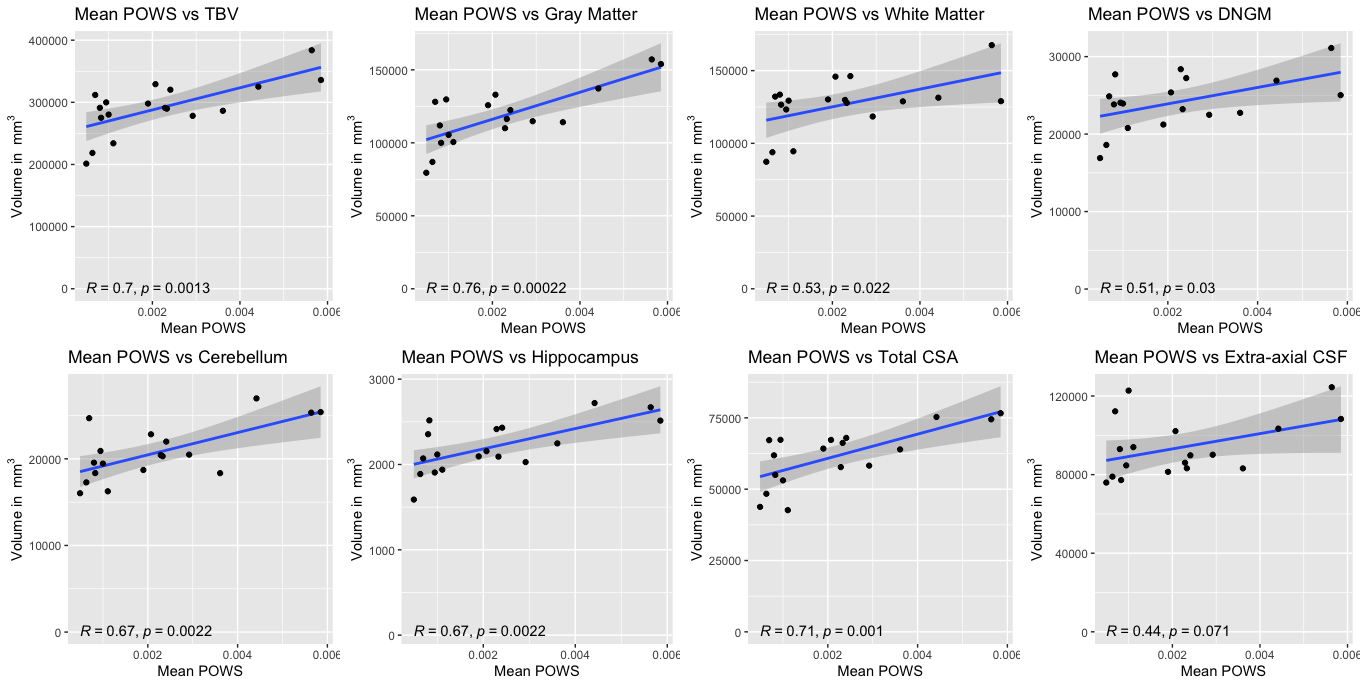
The relationship between the mean POWS score and regional brain volumes was assessed using simple linear regression and Pearson correlation. Generalized linear modeling was used to assess the strength of the relationship between POWS and brain volumes while controlling for gestational age at birth and known brain injury.
Results: 18 infants, with mean GA=25.8 weeks, mean BW=833g, and 50% female were included. Demographic/clinical factors are shown in Table 1. Mean POWS score strongly correlated with brain growth across regions (Figure 2), with the strongest relationship between POWS and gray matter volume. This relationship remained statistically significant, even when controlling for birth GA and other brain injury.
Conclusion(s): POWS summarized over the NICU course correlates with brain growth at term-equivalent age, independent of birth GA and brain injury. This novel physiologic metric may serve as a biomarker of the cumulative effect of stress and inflammation on early brain growth and development.