Emergency Medicine
Session: Emergency Medicine 8: Mental Health
584 - Optimizing pediatric patients' attainment of outpatient mental health services following emergency department care
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 584
Publication Number: 584.1909
Publication Number: 584.1909

Narmeen I. Khan, MD (she/her/hers)
Fellow Physician
Children's Hospital of Wisconsin
Wauwatosa, Wisconsin, United States
Presenting Author(s)
Background: A major contributing factor to the rise in emergency department (ED) mental and behavioral health (MBH) visits is the lack of accessible outpatient mental health services available, causing the ED to serve as a safety net. At our tertiary pediatric hospital, our MBH navigator follows up with patients to coordinate treatment plans with families.
Objective: To assess outpatient MBH care after discharge from the ED by (1) investigating the types of follow-up care patients with MBH concerns receive and (2) understanding facilitators and barriers that caregivers encounter in their efforts to obtain outpatient resources.
Design/Methods: This was a mixed methods study. We reviewed data collected as part of ongoing quality improvement efforts from 8/2021 to 9/2022 for patients aged 3 to 17 years seen at our ED for MBH concerns, received a social work consult, and contacted 1 week after the ED visit. Descriptive data included types of outpatient care received. Univariate logistic regression analyses were conducted with covariates including age, sex, race, Ask Suicide-Screening Questions (ASQ) scores, and repeat ED visit within 30 and 60 days. Multivariate analyses were performed for statistically significant results.
Additionally, we interviewed caregivers 4 weeks after the initial ED encounter to explore facilitators and barriers to obtaining outpatient care. Patients who returned to the ED for MBH concerns prior to the interview were excluded, amongst other factors. Content analysis for themes was then performed.
Results: The navigator successfully reached 533 out of 720 (74%) of patients. Of these, 83.3% were teenagers and 72.6% female. White was the most common race (58.5%) followed by black (30.6%). Most patients were unable to obtain follow-up MBH care.
Results from univariate regression analyses revealed that being white, having commercial insurance, and positive ASQ had higher odds of receiving intensive outpatient care (p < 0.05). Multivariate analyses found none of these 3 variables statistically significant when modeled together (Table 1).
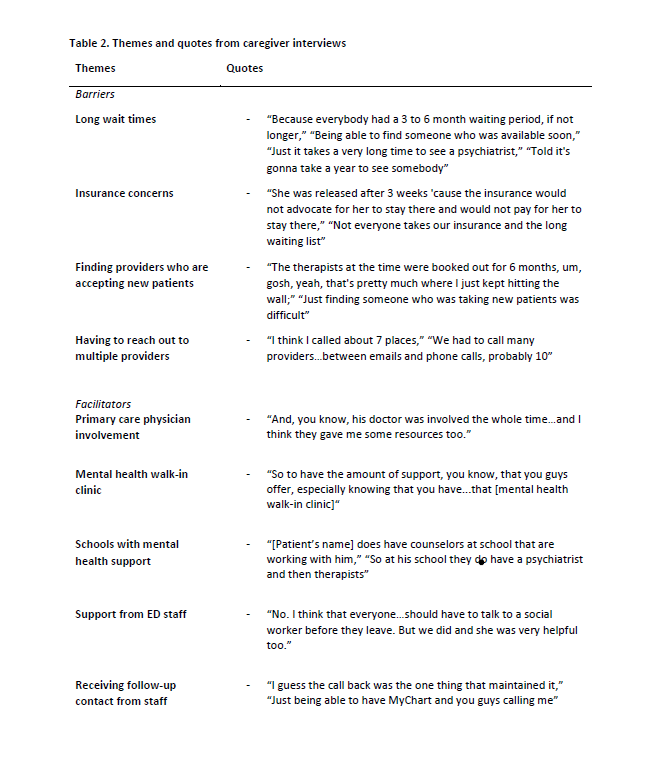
Facilitators to follow-up care noted by caregivers included support from ED staff and close relationships with primary care physicians. Barriers included long wait times and expense (Table 2).
Conclusion(s): Both our quantitative and qualitative work highlight racial and socioeconomic disparities that influence follow-up MBH care. Our findings shed light on challenges patients face in obtaining outpatient mental health care, serving as a valuable guide for directing efforts to improve the transition of ED-to-outpatient care.
.png)