Neonatology
Session: Neonatal Pulmonology - Clinical Science 2: Lung Imaging, Lung Function
205 - Identifying Optimal Positive End Expiratory Pressure (PEEP) in Neonates with Severe Bronchopulmonary Dysplasia with Electrical Impedance Tomography
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 205
Publication Number: 205.3103
Publication Number: 205.3103
Jessica E. Shui, MD (she/her/hers)
Neonatologist
MassGeneral Hospital for Children
Boston, Massachusetts, United States
Presenting Author(s)
Background: Little guidance exists for optimal ventilator positive end expiratory pressure (PEEP) strategies in infants with bronchopulmonary dysplasia (BPD), a chronic heterogenous lung disease due to abnormal lung development. Respiratory management in these infants is challenging because variable regional compliance can result in atelectasis of diseased lung tissue and overdistention of developing, healthier lung tissue. Ideally, ventilator setting goals strike the balance of providing adequate pressure to ventilate stiff, diseased lung tissue while minimizing volutrauma in healthy lung tissue to reduce progression of BPD. Current tools do not measure regional ventilation or regional compliance in heterogenous lung disease. In adults, electrical impedance tomography (EIT) has been used to provide these measurements non-invasively at the bedside to identify optimal PEEP. We report a novel application of EIT-guided PEEP titration in four infants with severe BPD.
Objective: 1) Validate EIT-guided PEEP titration in infants with heterogenous lung disease compared to infants with healthy lungs 2) Monitor duration of clinical tolerance of EIT guided ‘optimal PEEP’ settings.
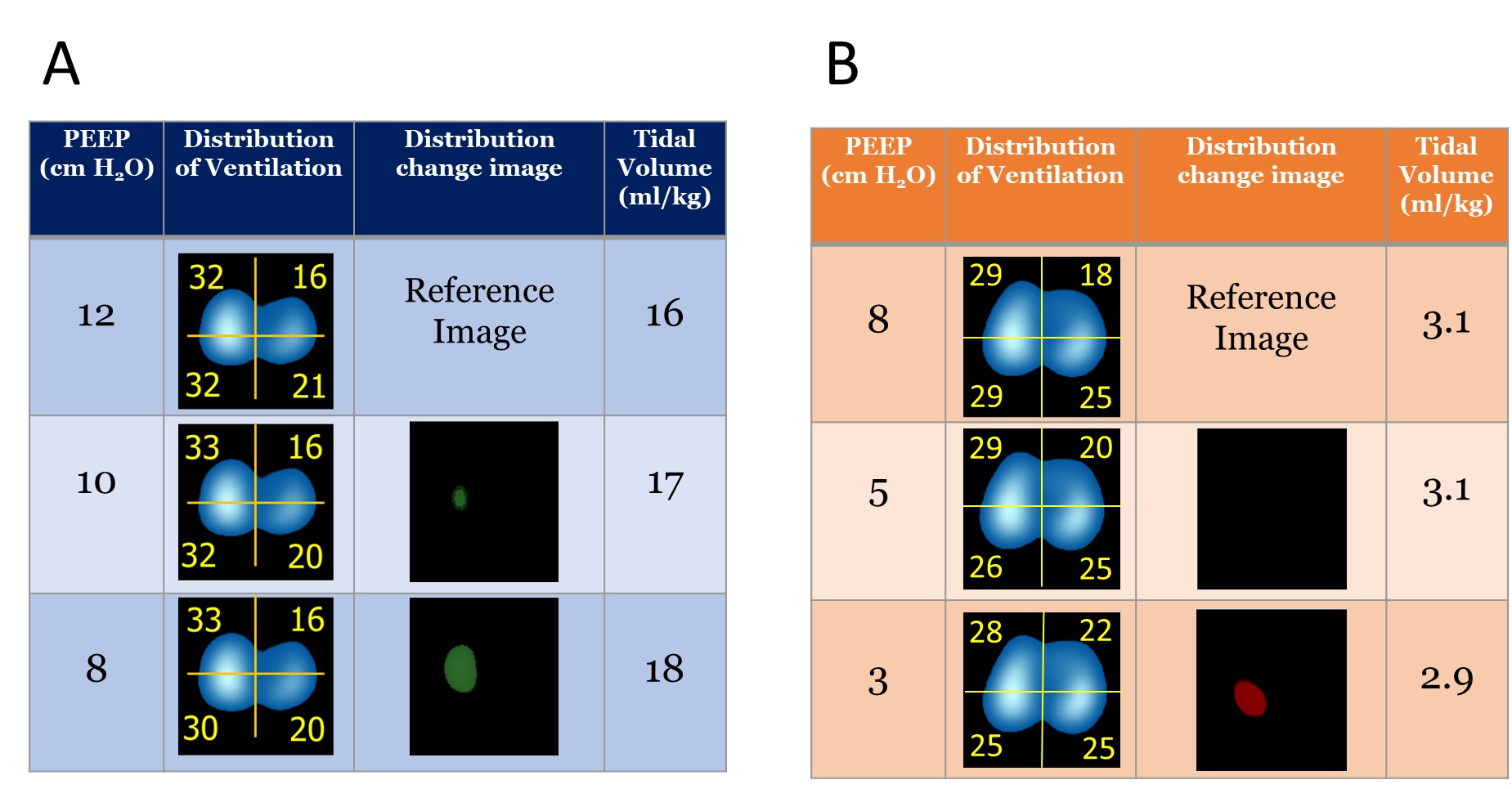
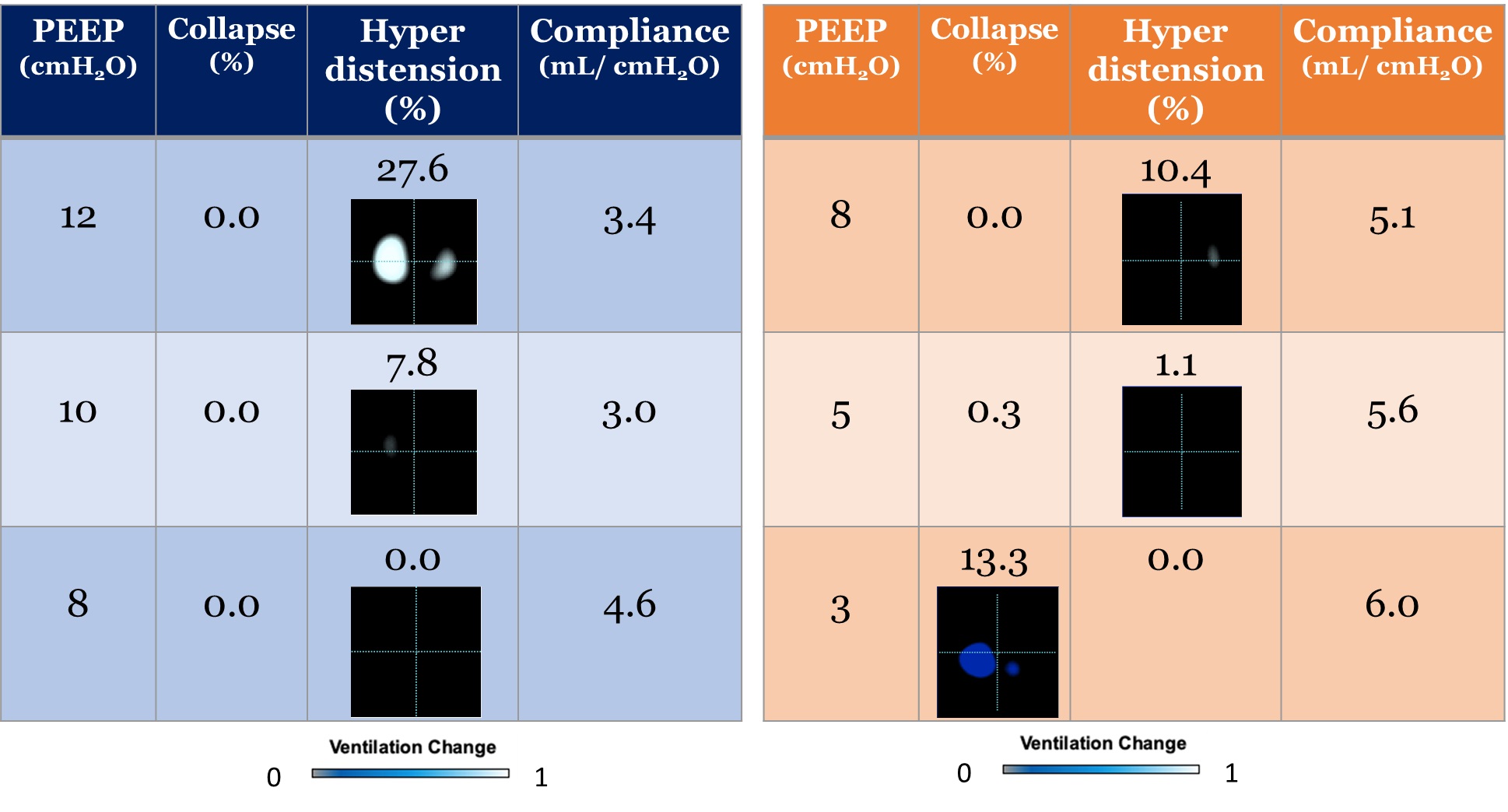
Design/Methods: This is a single-center, prospective case series from 8/2022-10/2023. An Enlight 2100 (Timpel Medical) belt was wrapped around the chest at T4. Ventilator data, physiologic bedside data, and EIT parameters were measured. A gradual PEEP titration, in increments of 2 cm H2O, ended when there was evidence of atelectasis. When loss of ventilation was noted, PEEP was increased by 2 cm H2O.
Results: Three infants < 6 months old with severe BPD were found to have regional lung overdistension and were able to reduce their PEEP by 33% (about 4 cm H2O) and decrease their supplemental oxygen requirement (mean of 0.77 to 0.28). These ‘optimal PEEP’ settings were maintained for 7 months, 1.5 months, and 3 weeks. One infant with BPD was already supported on optimal PEEP settings before EIT assessment. All infants with BPD had at least 33% worse compliance (range 33-84% worse compliance) compared to two healthy intubated infant controls.
Conclusion(s): Each preterm infant’s severity of heterogenous lung disease is unique and a personalized medicine approach to tailor ventilator settings is feasible and safe with EIT. EIT-guided PEEP titration in preterm infants with BPD can augment current respiratory assessment strategies to provide gentler ventilation.
.jpg)