Emergency Medicine
Session: Emergency Medicine 11: Potpourri
417 - Racial and Ethnic Disparities in an Emergency Department-Based Influenza Vaccine Delivery Model
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 417
Publication Number: 417.3182
Publication Number: 417.3182

Courtney D. Nelson, MD (she/her/hers)
Doctor
Nemours Children's Hospital
Wilmington, Delaware, United States
Presenting Author(s)
Background: Pediatric influenza causes significant morbidity and mortality. There are known racial and ethnic disparities in morbidity due to influenza, as well as influenza vaccine uptake. In the 2020-2021 influenza season vaccination rates in the United States were lowest among black children followed by Hispanic children, and highest in children of other races followed by white children. The Emergency Department (ED) has great potential to provide influenza vaccination.
Objective: To describe racial and ethnic differences in influenza vaccine acceptance and administration in an ED-based vaccine delivery model.
Design/Methods: In 2020, a multidisciplinary team of ED nurses, physicians, educators, and analysts developed a vaccine delivery model whereby nurses screen for vaccine eligibility during triage and vaccines are administered by the nurse upon discharge from the ED. Vaccine delivery programs took place over 4 separate seasons: Feb 2020-March 2020; September 2020-June 2021; October 2021-June 2022; Sept 2022-March 2023. Eligible patients include those who have not received a flu vaccine that season, have no contraindications for the vaccine, and whose parents agree to them receiving the flu vaccine in the ED. Vaccine acceptance was defined as the percent of patients whose parents agreed to influenza vaccination in the ED among those who did not have an influenza vaccine that season. Vaccine administration is the percent of patients who received the vaccine among those who were eligible.
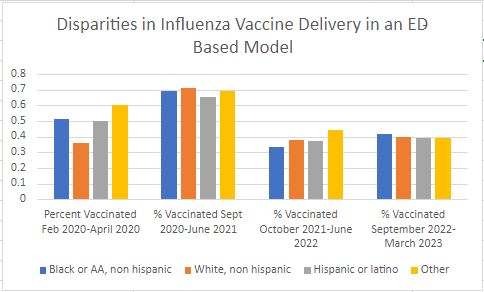
Results: There were 33,678 patients screened across all four seasons who had not received their influenza vaccine that season, and 4,782 (14.2%) parents agreed to have the influenza vaccine administered in the ED. There were 3,231 patients eligible for the flu vaccine and 1,608 received the flu vaccine (49.7%). There was significant difference in vaccine acceptance among racial and ethnic groups with Hispanic patients being the most likely to accept the influenza vaccine (16-28%), followed by patients classified as “other” (11-22%). Black, non-Hispanic patients were the least likely to accept the flu vaccine (9-15%) followed by white non-Hispanic patients (10-19%) (p-value < 0.0001). (Fig 1) There was no statistically significant difference in the rate of influenza vaccine administration among all groups (P-value >0.05, each season respectively). (Fig 2)
Conclusion(s): The ED provides an equitable environment for vaccine delivery and can help narrow vaccine disparities; however, influenza vaccine acceptance rates continue to mirror that seen in the general population.
.jpg)