Neonatology
Session: Neonatal-Perinatal Health Care Delivery: Practices and Procedures 3
473 - “Like a hot potato”: Disconnect in pediatric clinician perceptions of clinical utility of newborn toxicology testing and communication around testing with parents
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 473
Publication Number: 473.3251
Publication Number: 473.3251
Gina Liu, MSc (she/her/hers)
MD Student
Harvard Medical School
Allston, Massachusetts, United States
Presenting Author(s)
Background: Despite the common practice of newborn toxicology testing to assess perinatal substance exposure, few studies have explored how clinicians and birthing persons view the utility of newborn toxicology testing.
Objective: To understand the perspectives of newborn clinicians and birthing persons on the utility of newborn toxicology testing and communication around testing rationale and results.
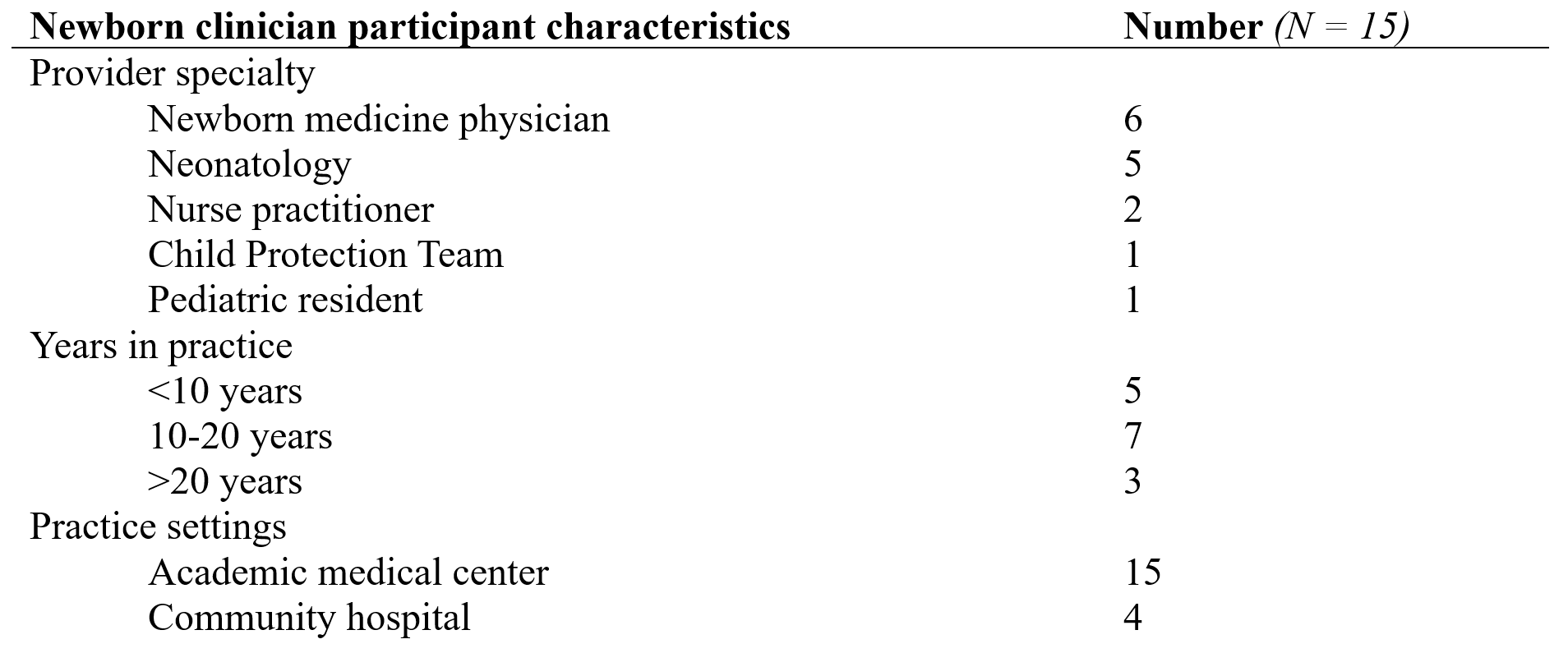
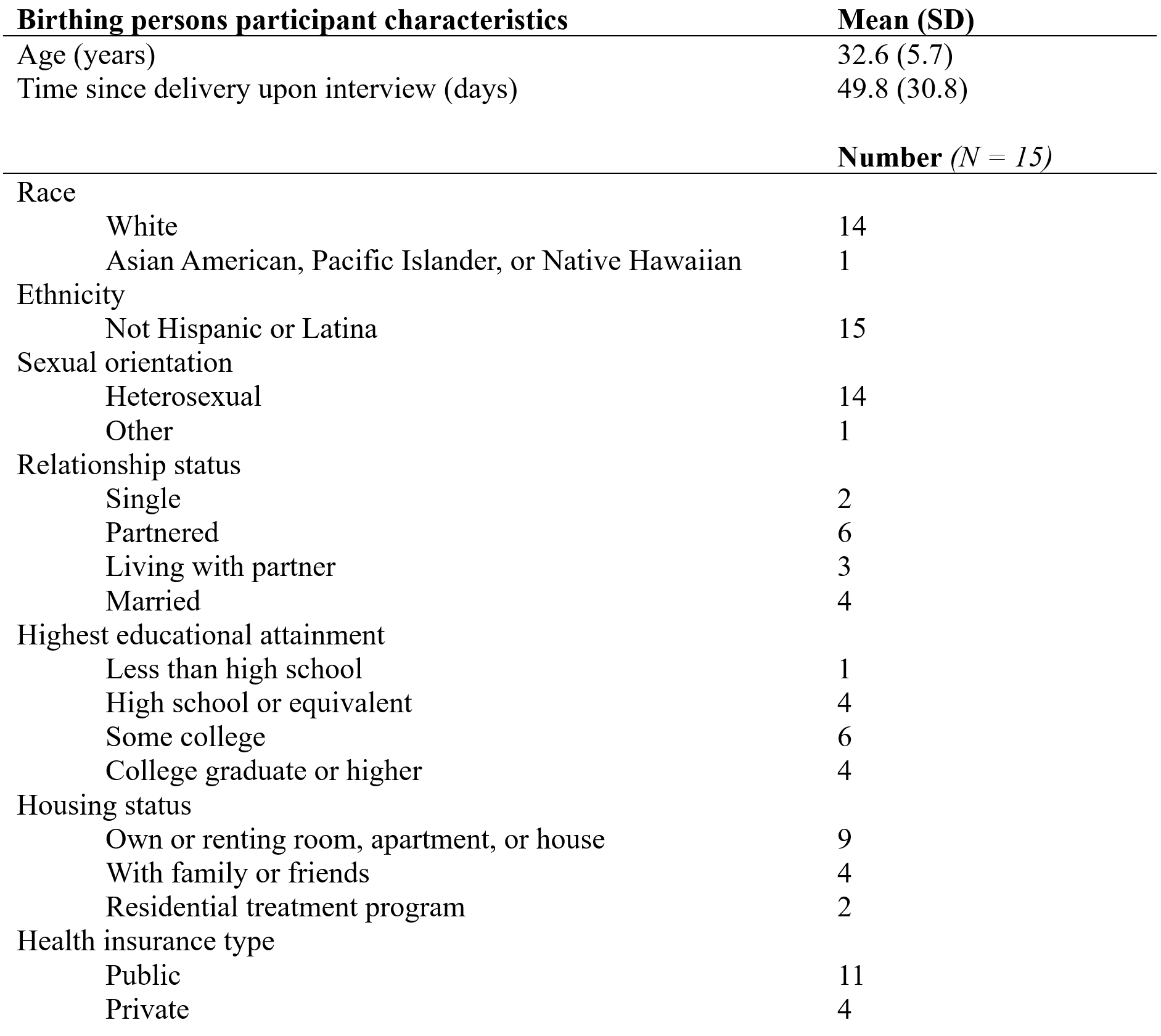
Design/Methods: Between April and November 2022, we conducted semi-structured interviews with 15 newborn clinicians involved in ordering toxicology testing and 15 birthing persons whose newborns underwent toxicology testing within a large health system in the Northeastern US. Clinician interviews explored indications, perceptions of utility, and attitudes toward parental consent for newborn toxicology testing. Birthing person interviews explored attitudes toward, knowledge of, and care team interactions with perinatal toxicology testing. Researchers open coded transcripts for clinician and birthing person interviews separately to generate two codebooks. Transcripts were then independently coded by two researchers with sufficient intercoder reliability and analyzed using a thematic analysis approach.
Results: We identified 5 themes across newborn clinician and birthing person interviews. 1) Clinicians described newborn urine toxicology testing as clinically useful for guiding neonatal opioid withdrawal syndrome management and preventing unnecessary diagnostic workup for certain neonatal clinical presentations. Most clinicians considered meconium testing to be primarily used for social risk assessment, but less clinically useful. 2) Many birthing persons had not received information about the clinical benefits and risks of newborn toxicology testing from a clinician. 3) Clinicians described fear of damaging the clinician-birthing person relationship and discomfort discussing potential child welfare involvement as factors negatively impacting communication around testing. 4) Birthing persons experienced confusion and misperceptions about the purpose of newborn toxicology testing when risk-benefit conversations were not held. 5) Birthing persons suggested structured consent conversations to correct this communication breakdown, while clinicians desired improved coordination across prenatal and perinatal care teams.
Conclusion(s): Despite clinicians frequently endorsing the clinical utility of newborn toxicology testing, clinical benefits were rarely discussed with birthing persons. Both birthing persons and clinicians offered suggestions for improving transparency and structure of toxicology testing discussions.
.png)