Neonatology
Session: Neonatal Neurology 3: Clinical
38 - Generalized Movements Assessment and Hammersmith Infant Neurologic Exam support early diagnosis of cerebral palsy in infants treated with therapeutic hypothermia for neonatal encephalopathy
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 38
Publication Number: 38.54
Publication Number: 38.54

Sara N. Moss, MD (she/her/hers)
Resident, PGY-2
University of Utah School of Medicine
Salt Lake City, Utah, United States
Presenting Author(s)
Background: Cerebral palsy (CP) is the most common motor sequela of neonatal encephalopathy (NE). Early diagnosis is imperative to allow for early intervention. The General Movements Assessment (GMA) and Hammersmith Infant Neurologic Exam (HINE) are validated tools for early CP detection and risk stratification in premature infants at risk for developmental delay. Several groups have explored GMA and HINE in small cohorts of infants with NE but have conflicting results, and evidence that the association between GMA and CP is abolished by therapeutic hypothermia (TH). Therefore, there is no clear evidence that performing GMA and HINE on cooled infants at 3 months of life provides diagnostic value. The center for neurodevelopmental follow up at the University of Utah has participated in the CP Early Detection initiative since 2018, with both GMA and HINE routinely administered to all infants who underwent TH for NE.
Objective: To examine the relationship between GMA, HINE, and risk of CP in a cohort of infants who have undergone TH in a large single center and establish if HINE and GMA support the early diagnosis of CP.
Design/Methods: This is a retrospective cohort study from a large single center that included surviving infants with moderate or severe NE who underwent TH between 2018-2023. GMA and HINE were initially assessed at 3 months of life by validated examiners and patients were followed for at least 12 months.
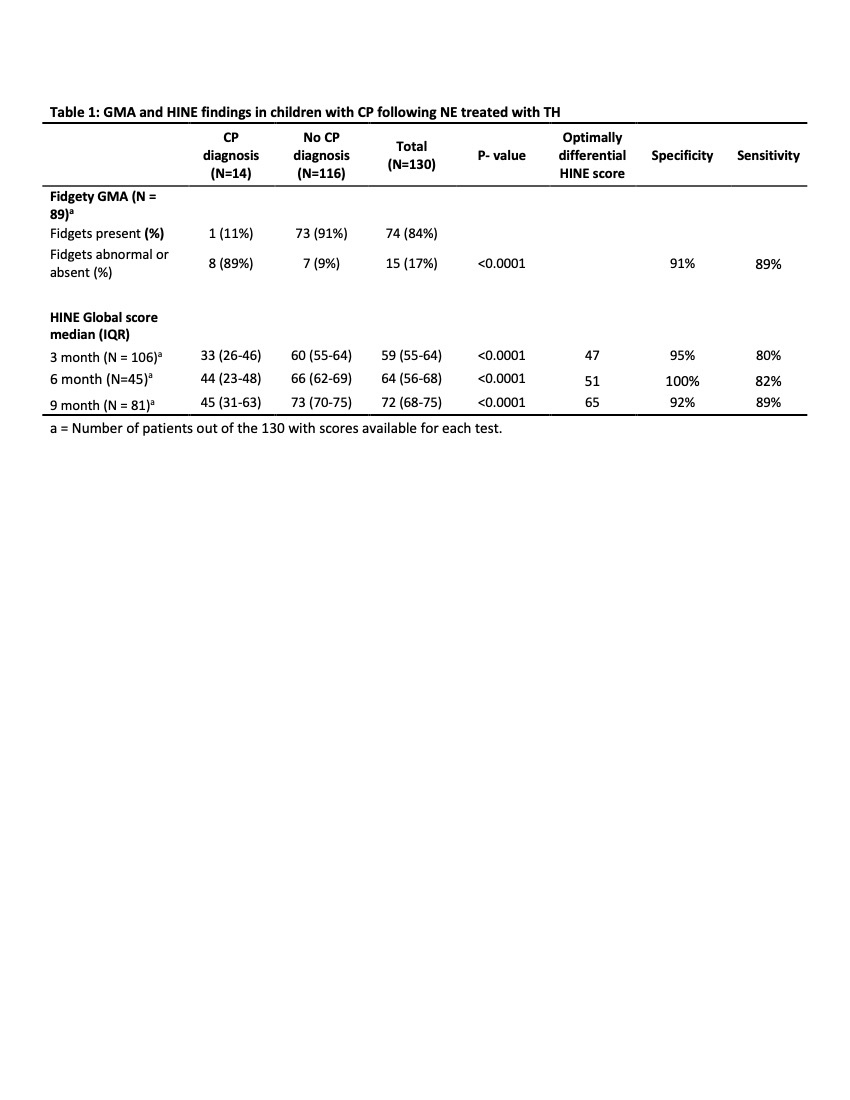
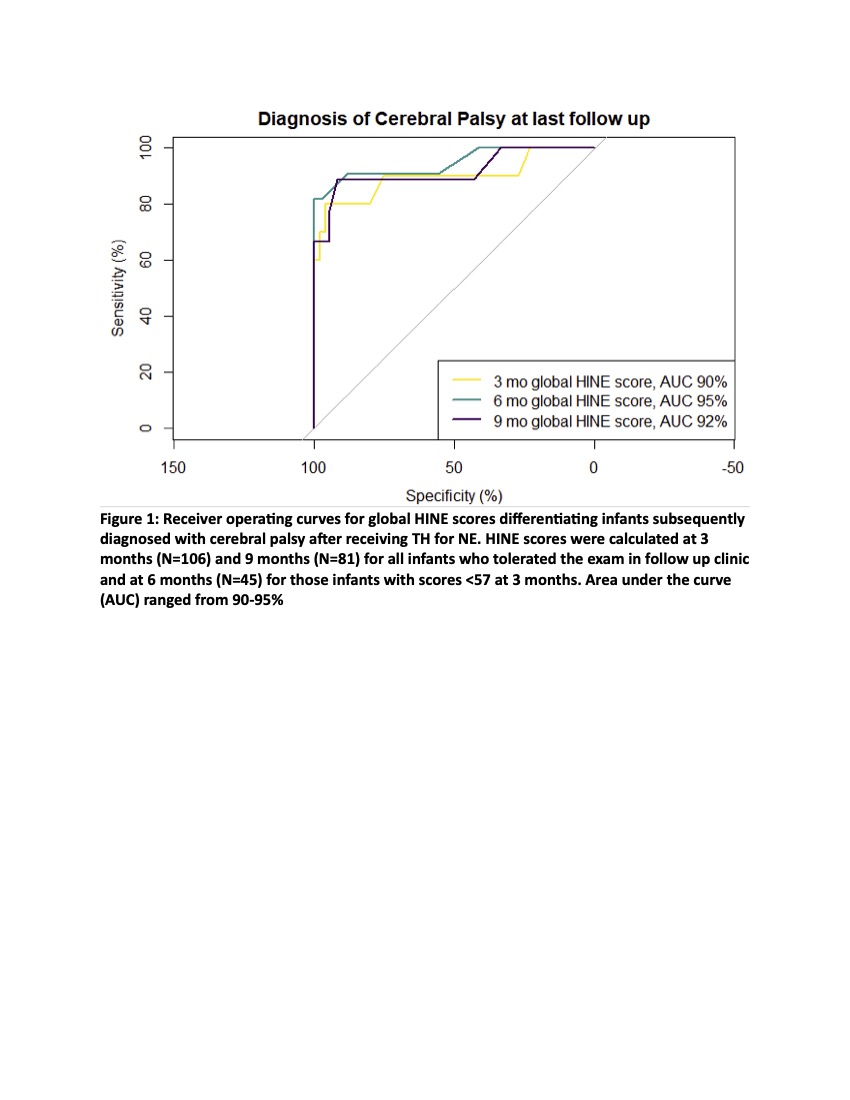
Results: Of 201 infants who underwent TH, 177 survived the initial hospitalization, and 72% (N = 130) were seen in follow-up. CP was diagnosed in 14 patients (11%). The absence of fidgety movements at the 3-month GMA was highly associated with CP (p-value = < 0.0001, sensitivity 89%, specificity 91%) (Table 1). Similarly, all HINE assessments were associated with CP at 3 months (p-value < 0.0001, sensitivity 80% specificity 95%), 6 months (p < 0.0001, sensitivity 82%, specificity 100%), and 9 months (p < 0.0001, sensitivity 89%, specificity 92%) with an area under the receiver operating curve ranging from 90% - 95% (Figure 1).
Conclusion(s): GMA and HINE were predictive of CP in term infants with NE who had undergone TH. The presence or absence of fidgets on GMA at 3 months and the HINE score at 3, 6 and 9 months were all highly associated with CP diagnosis with >80% sensitivity and > 90% specificity. The optimal HINE score for predicting CP may differ from premature infants and will benefit from further studies. Ongoing analysis will also include trajectory data for repeated HINE and GMA scoring, and evaluation of HINE and GMA combined to predict CP.