Neonatology
Session: Neonatal General 7: Respiratory
246 - A Retrospective Analysis of Extubation Success in a Level III NICU
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 246
Publication Number: 246.3319
Publication Number: 246.3319

Ann Chacko, DO (she/her/hers)
NICU Fellow
University of Wisconsin School of Medicine and Public Health
Madison, Wisconsin, United States
Presenting Author(s)
Background: Determining when to extubate an intubated neonate remains an ongoing challenge. Lack of standardized extubation guidelines requires clinicians to rely on available clinical, lab data, and subjective experience. Prolonged mechanical ventilation leads to increased risk of bronchopulmonary dysplasia and early extubation may provide protection from further neonatal lung injury. Therefore, it is imperative to determine factors that impact extubation success and reduce the frequency of reintubation.
Objective: Evaluate reintubation rates (reintubation within 72 hours versus after 72 hours) and factors influencing extubation success.
Design/Methods: Retrospective cohort study of infants at UnityPoint Health-Meriter Hospital Level III Neonatal Intensive Care Unit (NICU) from January 2022 to January 2023. Inclusion criteria included infants intubated due to respiratory distress, with exclusions for congenital anomalies or transfers to external hospitals. Data were analyzed with nonparametric methods and Fisher’s exact test.
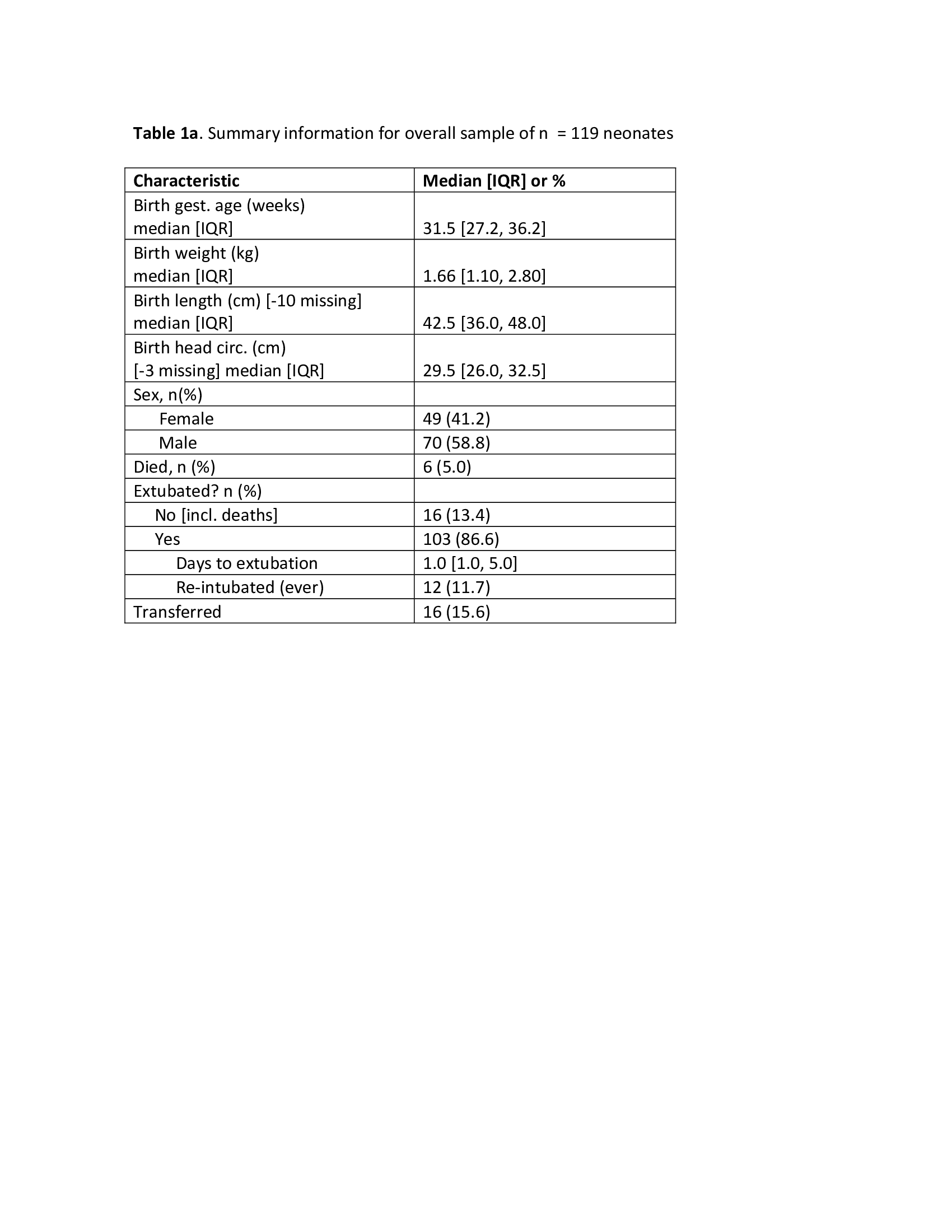
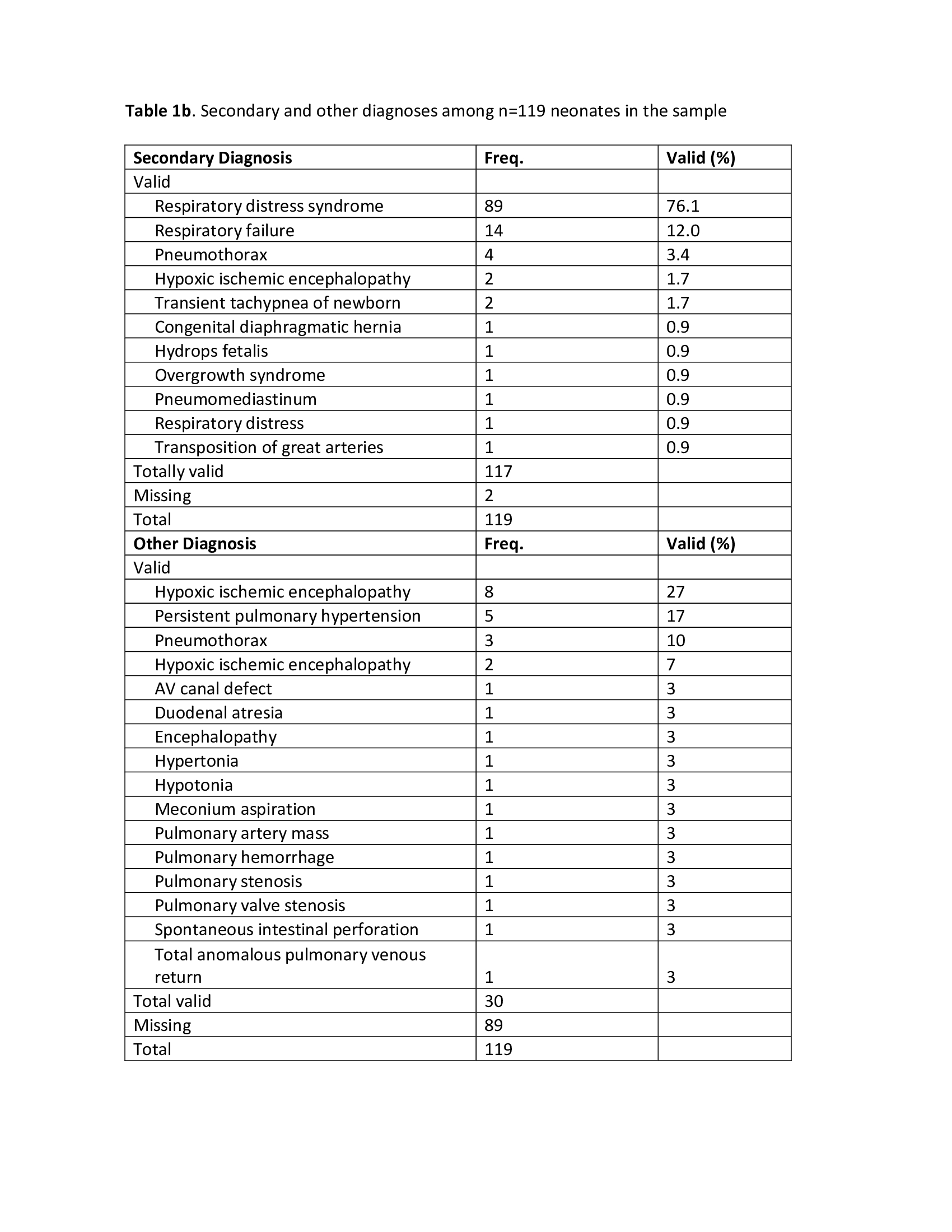
Results: Of 119 neonates, 103 met inclusion criteria and 12 (11.7%) required re-intubation (Table 1a). The median gestational age was 31.5 weeks with a corresponding median birth weight of 1.66 kg. All neonates had respiratory distress as their primary diagnosis while other diagnoses are detailed in Table 1b.
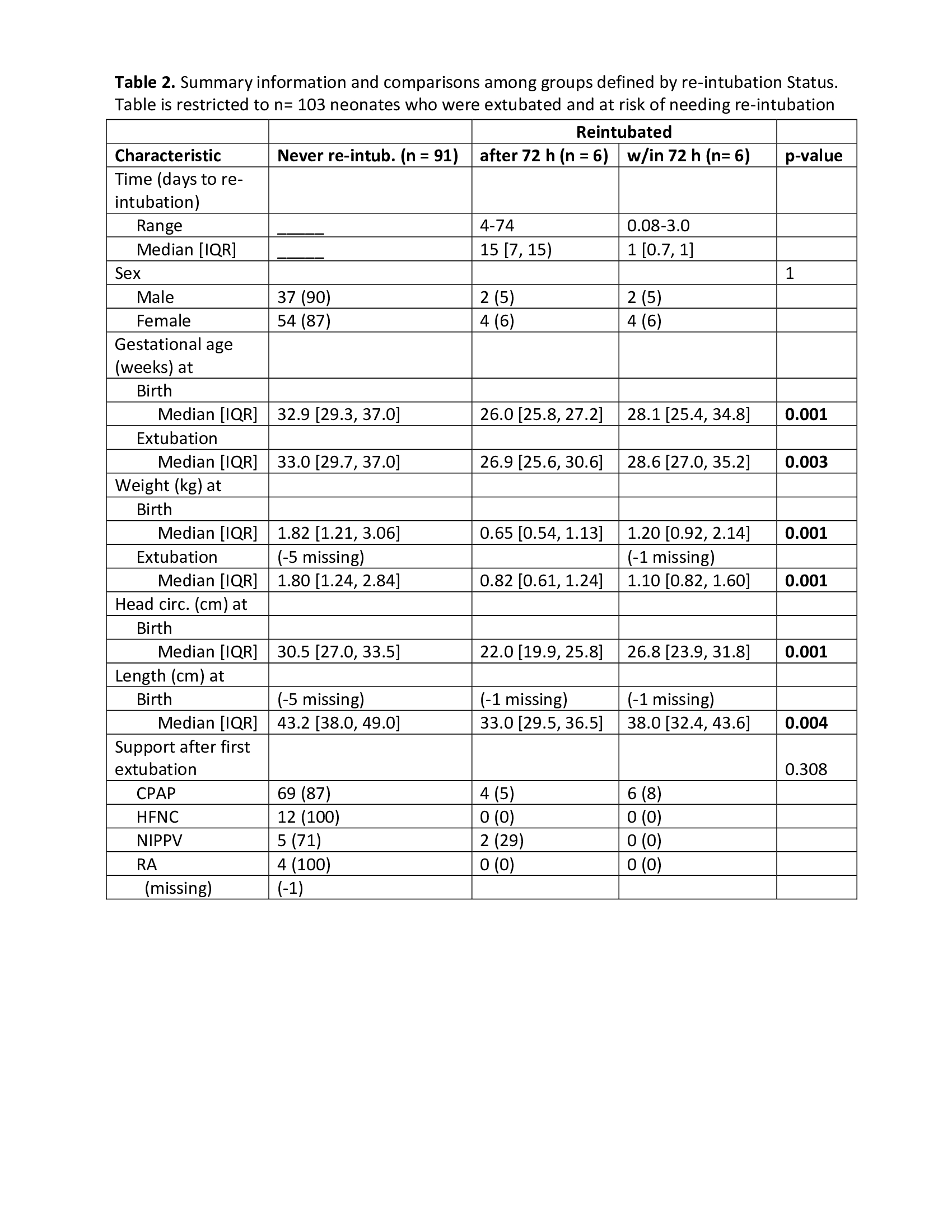
The 103 neonates were categorized by re-intubation time: never (n = 91), after 72 hours (n = 6), and reintubated at or before 72 hours (n = 6). Significant differences in age/size parameters were evident among the groups (p ≤ .004), but no distinction between early and late re-intubation (p > 0.15) was observed. Smaller / younger neonates had greater likelihood of reintubation (p ≤ .002). Post-extubation respiratory support did not correlate with re-intubation (p = .308). Mean airway pressure (MAP on CPAP after initial extubation) did not differ among the groups, with a median of 6 (Table 2).
Conclusion(s): Our study indicates a 12% re-intubation risk with results suggesting differences based on gestational age and size parameters. Younger and smaller infants had greater likelihood of re-intubation. While the study did not identify differences in reintubation rates between early and late re-intubation, close monitoring of all neonates post-extubation is vital regardless of timing. Furthermore, post-extubation respiratory support was not a significant predictor of re-intubation. These findings contribute to the ongoing development of effective neonatal extubation strategies.