Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 5
37 - Tech It to the Next Level: A Quality Improvement Project to Improve Diabetes Technology Education for Pediatric Resident Physicians
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 37
Publication Number: 37.2998
Publication Number: 37.2998

Madeline F.E Parr, MD (she/her/hers)
Resident
Joseph M. Sanzari Children's Hospital Hackensack University Medical Center
Hackensack, New Jersey, United States
Presenting Author(s)
Background: Due to a growing shortage of pediatric endocrinologists, pediatricians require a strong knowledge of diabetes management. Insulin pumps and continuous glucose monitors are increasingly used for type 1 diabetes; thus pediatricians need to be proficient with the latest advancements. Recent data from the Type 1 Diabetes Exchange Data shows 57% of children aged 0-13 years old and 75% of children aged 13-17 use an insulin pump. Our prior Plan-Do-Study-Act (PDSA) cycle demonstrated overall improvements in pediatric resident comfort and knowledge in diabetes management but with continued education gaps related to diabetes technology with 82% of residents expressing discomfort in pump management. Thus, in this second cycle, we developed a novel, resident-championed curriculum to promote proficiency with diabetes technology.
Objective: To increase resident self-reported measures of comfort with diabetes technology by 15% and to improve accuracy on assessment questions by 15% related to diabetes technology within 6 months.
Design/Methods: This quality improvement (QI) initiative used the PDSA cycle method. Stakeholders included residents, nurses, endocrinologists, and advanced practice providers. This cycle’s interventions included the creation of a tip sheet focused on diabetes technology, teaching sessions with clinical cases and active participation with interactive polling technology, hands-on practice with device administration, and insulin pump simulator phone applications. Outcome measures were resident comfort using Likert scales and objective knowledge using multiple choice questions in pre- and post-surveys. Statistical analysis was performed using McNemar’s and paired t-tests in Python.
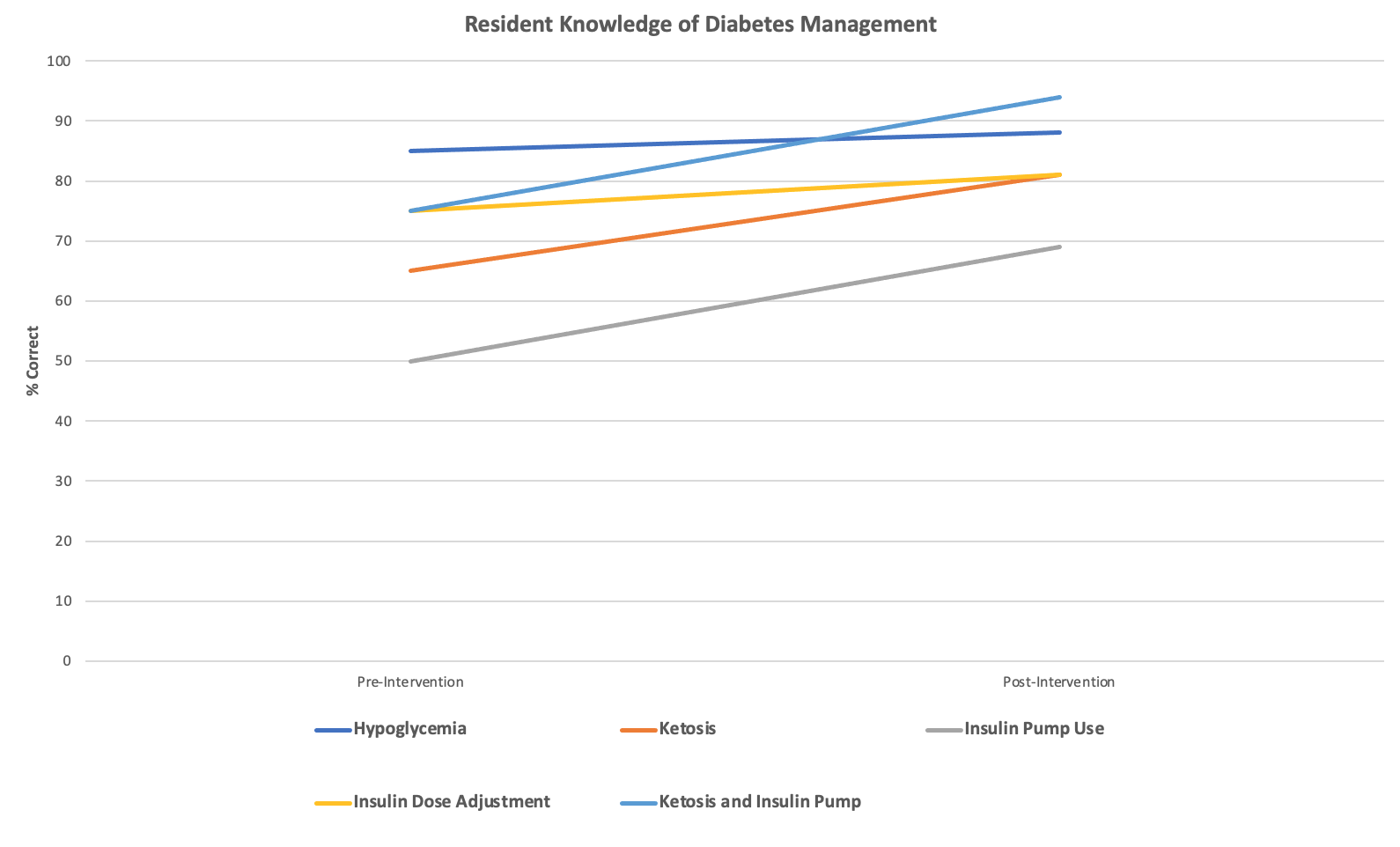
Results: Resident comfort improved for reviewing insulin pump settings (20% to 69%, p< 0.05), insulin pump use (20% to 69%, p=0.06), and continuous glucose monitoring (30% to 63%, p=0.06). With regards to objective knowledge questions, diabetes knowledge assessment scores rose from 70% to 85%. There was an increase in percentage correct for questions related to insulin pump use (50% to 69%) and ketone management on pumps (75% to 94%).
Conclusion(s): This QI project sustained previous resident comfort and knowledge in diabetes management with focused emphasis on improving knowledge gaps related to diabetes technology. Our future efforts will include system-level change to implement an inpatient diabetes clinical care pathway based on stakeholder feedback and incorporating the latest clinical evidence, including advances in technology.
.png)
