Emergency Medicine
Session: Emergency Medicine 1: Operations and Research
363 - Adverse Safety Events Among Pediatric Emergency Medical Services Encounters With and Without a Pediatric Emergency Care Coordinator
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 363
Publication Number: 363.469
Publication Number: 363.469
- MC
Mark X. Cicero, MD
Associate Professor
Yale University School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background: Pediatric emergency medical services (EMS) encounters are infrequent, with the majority being low-acuity and with the majority being low acuity minimal interventions. This infrequency contributes to adverse safety events (ASEs), yet the frequency and kinds of ASEs in pediatric EMS are not well characterized.
Objective: To evaluate the frequency and type of ASEs in pediatric EMS encounters.
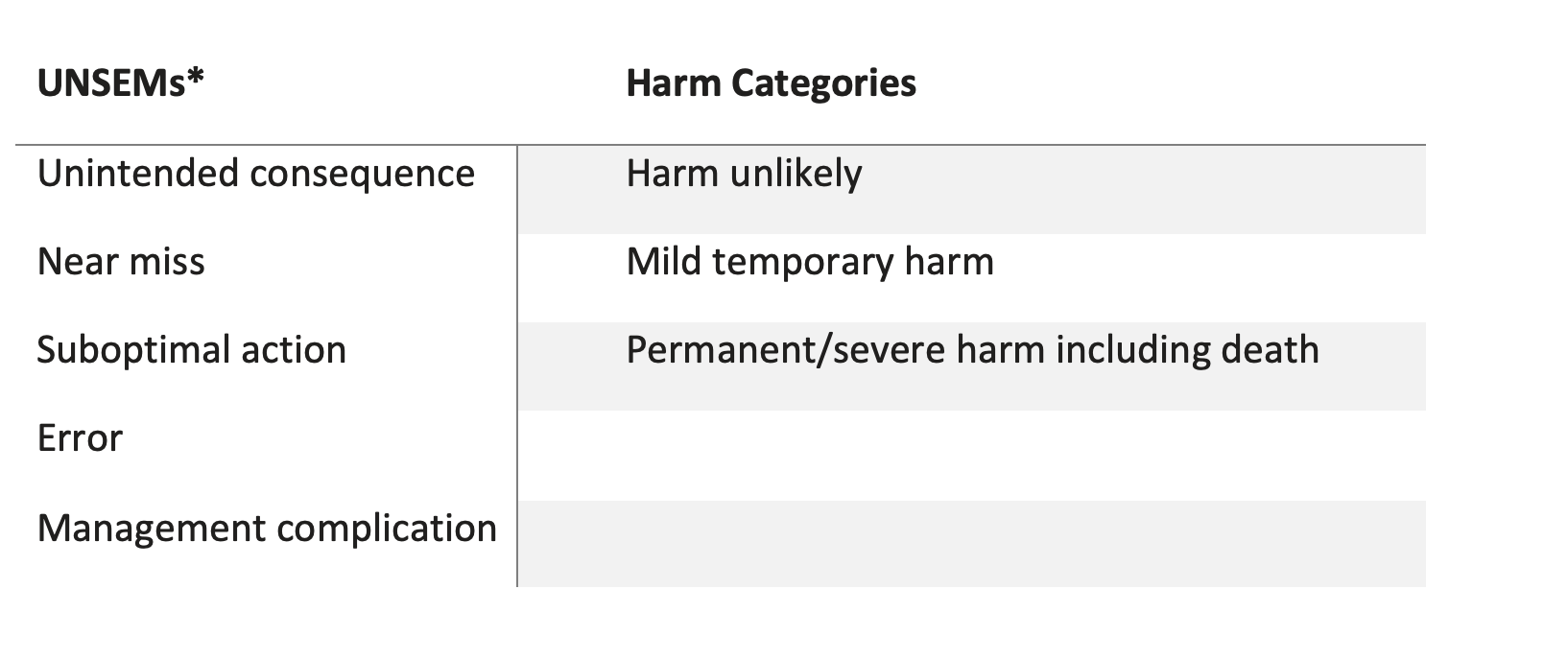
Design/Methods: EMS patient encounters and associated emergency department (ED) records for patients < 18 years of age were reviewed. The primary outcome was the frequency of ASEs in five clinical interventions (evaluation, medication, fluids, procedures, and assessment). ASEs were categorized across five types of outcomes (UNSEMs) using a previously validated chart extraction rubric for pediatric EMS care (Table 1). Frequency of documented EMS clinical interventions and procedures were quantified and recorded as percentages. Preliminary data are reported from EMS agencies within two states.
Results: In review of 594 pediatric EMS encounters with ED visits, mean age was 12 years (range 1 day - 17.9 years), with 47.2% admitted to the hospital. ASEs occurred in all clinical categories, most frequently with procedures, performed for 291 patients with 100 identified ASEs (34.4%), the most frequent UNSEMs were Errors (n = 47, e.g., failure to apply splint or c-collar) and Management Complications (n = 41, e.g., unsuccessful IV placement) . Evaluation-related ASEs occurred for 98 patients. The most common UNSEM for Evaluation was associated with the physical exam with suboptimal actions reported for 94 patients, most frequently incomplete physical exam (e.g. no neurological exam for a reported head injury). The least common involved Fluids, administered in 141 patients with 8 identified ASEs (5.8%) (e.g., too little fluid administered by body weight), the most frequent Fluids UNSEM was near miss (n = 3). 208 patients were administered medications during the transport, ASEs were occurred for 19 patients (9.1%) (e.g., underdose or overdose of medications), the most frequent UNSEM (n = 10) was unintended consequences. Resuscitation protocols were used for two patients, with no documented ASEs. Most ASEs were determined to be ‘harm unlikely’ (68%).
Conclusion(s): ASEs occurred frequently in a cohort of pediatric EMS encounters, particularly when patients had procedures. Next steps include comparing ASES and UNSEMs in EMS agencies with and without pediatric emergency care coordinators (PECCs), to determine if the presence of a PECC is associated with frequency and types of ASEs.
.png)
