Neonatology
Session: Neonatal/Infant Resuscitation 2
278 - Umbilical Cord Pulse Oximetry - Could it help guide delaying the clamping of the umbilical cord, and predict the accurate heart rate and oxygen saturation in the delivery room?
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 278
Publication Number: 278.2746
Publication Number: 278.2746

Praveen Chandrasekharan, MD, MS (he/him/his)
Associate Professor of Pediatrics
Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo
Buffalo, New York, United States
Presenting Author(s)
Background: Until electrocardiogram (ECG) was introduced in the delivery room, pulse oximetry placed on the right hand of a newborn (preductal) was used to record both the heart rate (HR) and oxygen saturation (SpO2). To date, these two parameters help guide us to the next steps of resuscitation in the delivery room (DR). Sjoding et al. (NEJM 2020) have highlighted racial bias in pulse oximetry measurement. To overcome this issue, although umbilical cord pulse oximetry is post-ductal, it could help predict the umbilical flows, HR & SpO2.
Objective: To evaluate the use of umbilical cord pulse oximetry in a preterm asphyxiated ovine model.
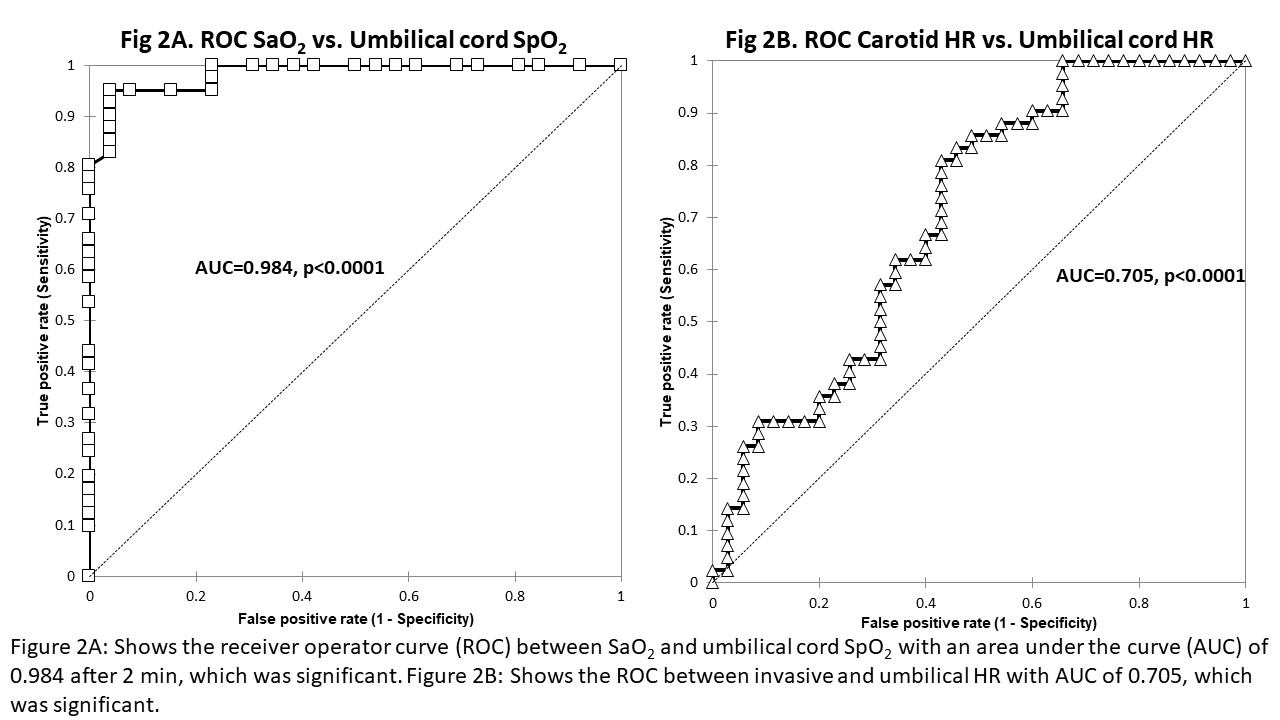
Design/Methods: Post instrumentation and asphyxia by umbilical cord occlusion until HR < 100 bpm, we used five preterm lambs (126-129d) and applied NONIN pulse oximetry to the umbilical cord and on the right forelimb/tongue to record preductal saturations. HR was invasively measured using carotid blood flows. Supplemental oxygen was started at 60% and titrated after 2 min based on preductal goals every minute as recommended by NRP. Ventilation was monitored using NM3 Philips monitor and tidal volume was maintained between 8 -10 ml/kg. Oxygen saturation of the arterial blood (SaO2) was measured. A receiver operator curve (ROC) was evaluated using invasive HR (from the carotid line) and SaO2 against umbilical pulse oximetry after a minute (from 2 min onwards).
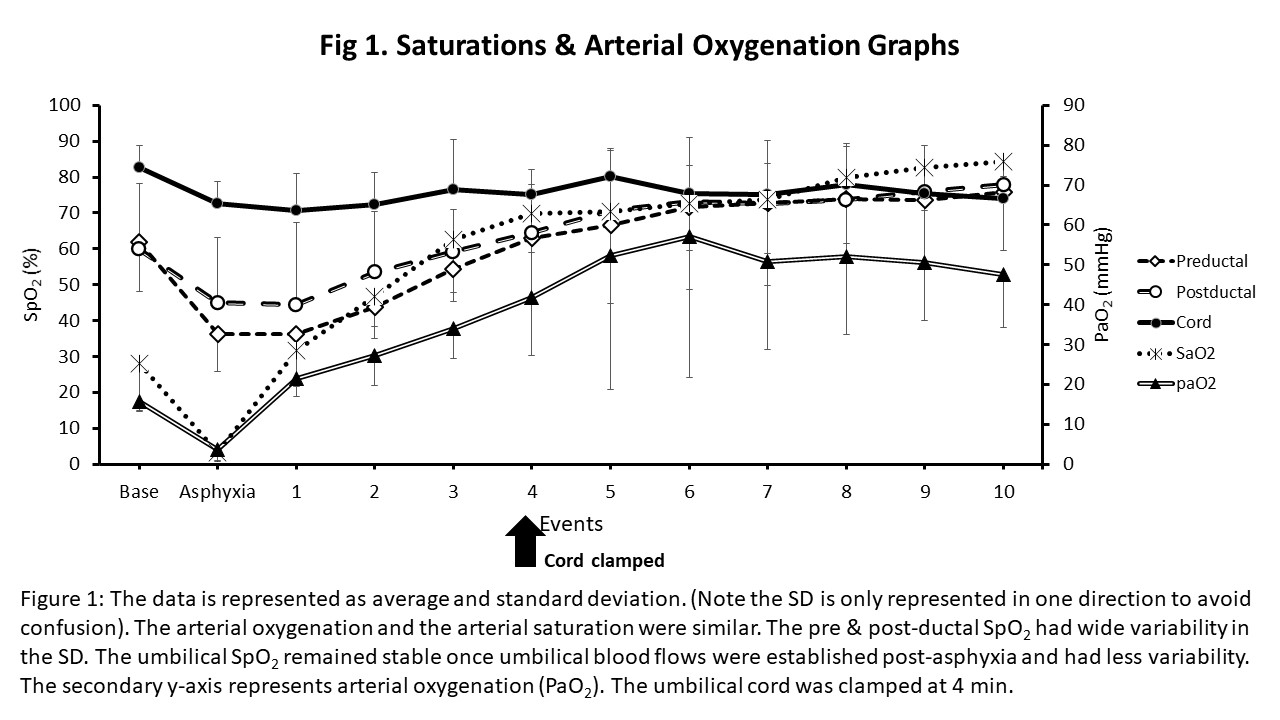
Results: The five preterm lambs post asphyxia (HR < 100bpm) underwent a delay in the clamping of the umbilical cord for 4 min. The flows to the umbilical cord continued despite clamping. Figure 1 shows the pre & post ductal SpO2, SaO2, and arterial oxygenation (PaO2) for the first ten min. Pre & post ductal SpO2 had wide standard deviations in the first few minutes post-asphyxia. Fig 2 shows the receiver operator curve (ROC) between SaO2 and umbilical SpO2 (fig 2A) and carotid arterial HR and umbilical HR (fig 2B), which were significant. In the first 4 min (fig 3), the umbilical venous (UV) and arterial (UA) flow were not different. After 4 min, the umbilical cord was clamped, but we noticed perfusion/pulsations.
Conclusion(s): Umbilical pulse oximetry could be a useful tool to predict SpO2, HR, and umbilical blood flow accurately. Although post-ductal, since no skin is involved, placing pulse oximetry around the umbilical cord could overcome the skin pigmentation issue and be readily translated into the human newborn. Furthermore, this will avoid excess oxygen exposure and help decide the duration to clamp the umbilical cord.
.jpg)
