Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 6
53 - Safeguarding Healthcare Heroes: Unmasking the Realities of Employee Safety Events
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 53
Publication Number: 53.2773
Publication Number: 53.2773

Ann Kane, MD (she/her/hers)
Medical Director of Quality
Johns Hopkins Children's Center
Silver Spring, Maryland, United States
Presenting Author(s)
Background: Patient behavioral events, such as aggression, verbal abuse, assaults, elopement, and self-harm, pose substantial risks to both patients and healthcare staff, with potential consequences ranging from physical to emotional and psychological harm. A workgroup was formed to pilot the data collection process in our inpatient pediatric psychiatric unit.
Objective: Our primary objective was to comprehensively investigate and understand the contributing factors of patient behavioral events within the context of a growing number of staff safety incidents and behavioral health patients. By using various QI tools and methodologies, the goal was for the patient care team to gain a comprehensive understanding of this critical issue, enabling informed decision-making to enhance staff and patient safety.
Design/Methods: We started with a swimlane to visualize how we report patient behavioral events leading to staff harm, uncovering bottlenecks and process gaps. Our Ishikawa diagram categorized underlying causes like people-related factors and environmental conditions as contributing factors. Data collection involved incident reports, historical data, and a nursing staff survey to quantify event frequency, staff expectations, and reporting experiences for future improvement. This comprehensive approach aims to establish trends, facilitating continuous improvement efforts.
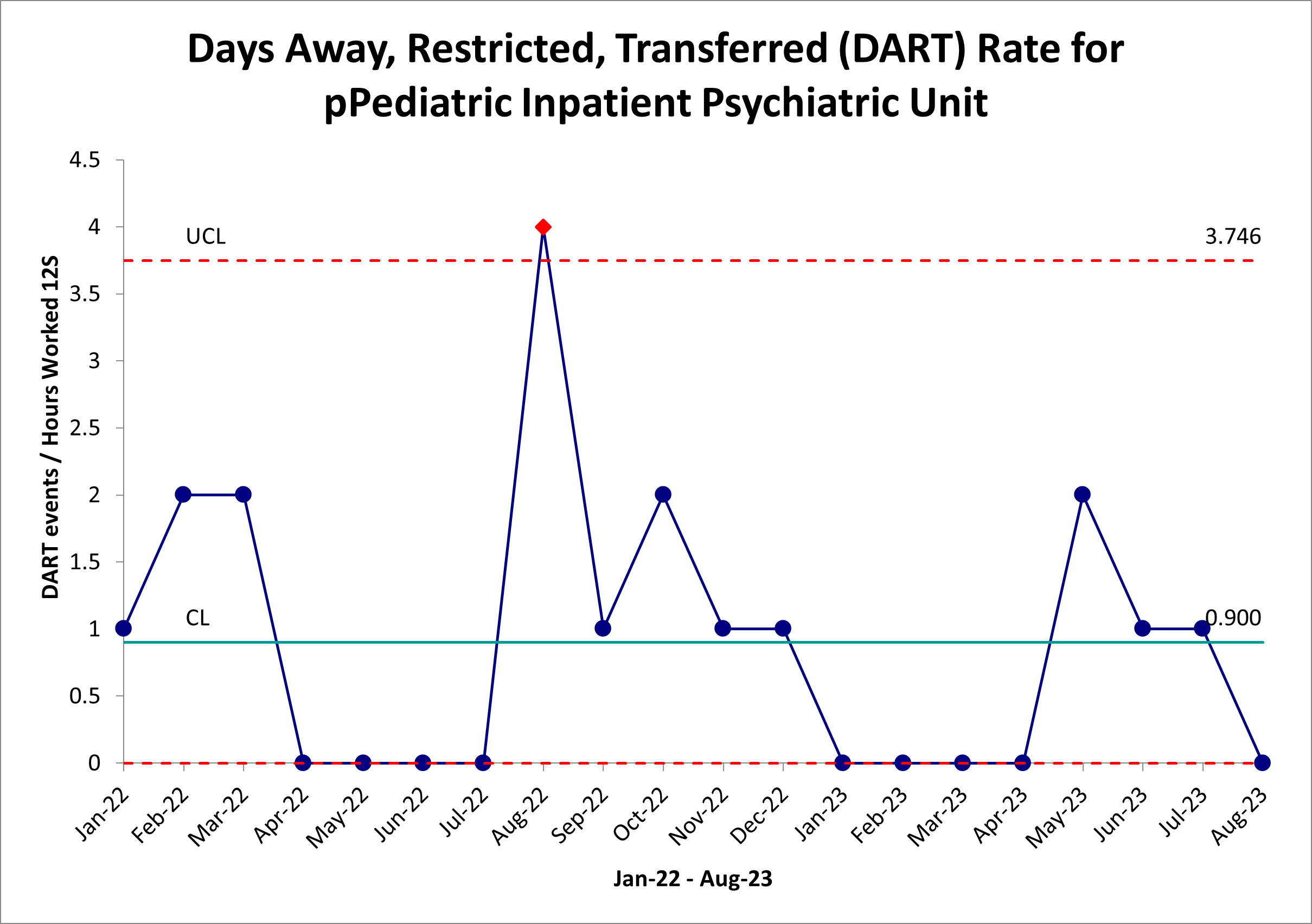
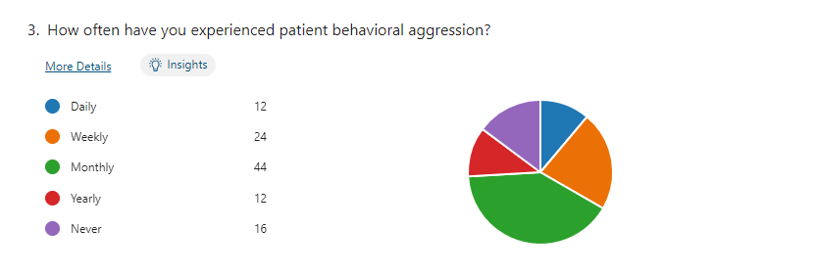
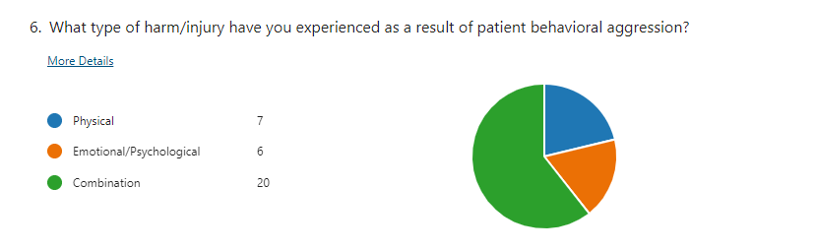
Results: In 2022, Employee/Staff Safety (ESS) incident reports accounted for 5% (n=176) of all events at Johns Hopkins Children’s Center (JHCC). Patient Behavioral ESS events accounted for 64% (n=107) in our inpatient psychiatric unit, resulting in a Days Away, Restricted, Transferred (DART) rate of 20.4 for calendar year 2022. Initial responses from the nursing survey revealed 18% (n=20) of respondents experience a combination of physical and emotional/psychological harm. Respondents also indicated their experience with patient aggression occurs weekly and monthly, 22% and 40% respectively. Qualitative analysis suggests reporting barriers include lack of awareness, desensitization to harm, and previous negative experiences, all of which contribute to our potential gap in DART data.
Conclusion(s): Further review of our nursing staff safety survey is warranted, however, initial findings indicate the following opportunities for improvement: evaluation of reporting culture to injury clinic, evaluation of Safety Cares de-escalation training effectiveness, and improved staff education and awareness. Additionally, we aim to widen the scope of our workgroup to encompass all units as well as include security personnel.