Neonatology
Session: Neonatal General 7: Respiratory
247 - Accuracy of the online Extubation Success Calculator (ExSC) in predicting preterm infants’ extubation readiness
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 247
Publication Number: 247.2808
Publication Number: 247.2808
- KN
Khang Nguyen, MD (he/him/his)
Resident physician
Einstein Jefferson Hospital
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Invasive mechanical ventilation in preterm infants is not without complications; thus, the goal is to extubate as early as possible. Determining extubation readiness is critical, as unsuccessful extubation can lead to BPD, prolonged hospital stay, and increased mortality. The Web-based Extubation Success Calculator may be a valuable tool for guiding extubation decisions in preterm infants.
Objective: (1) Evaluate the ability of ExSC to predict extubation readiness in preterm infants. (2) Determine if there is an optimal threshold ExSC probability that correlates with successful extubation.
Design/Methods: A retrospective study of intubated infants with a gestational age (GA) ≤32 weeks admitted between February 2019 and January 2023 in a level III NICU. Electronic medical records were abstracted for demographics, morbidities, medications, blood gases, and ventilator settings. ExSC and pre-extubation Ventilation Index (VI) were computed for all extubations. All infants were on caffeine and extubated to non-invasive support. Failed extubation was defined as the need for reintubation within 5 days of extubation. Chi-Square, Student's t-test, and a uni/multivariate logistic regression were calculated.
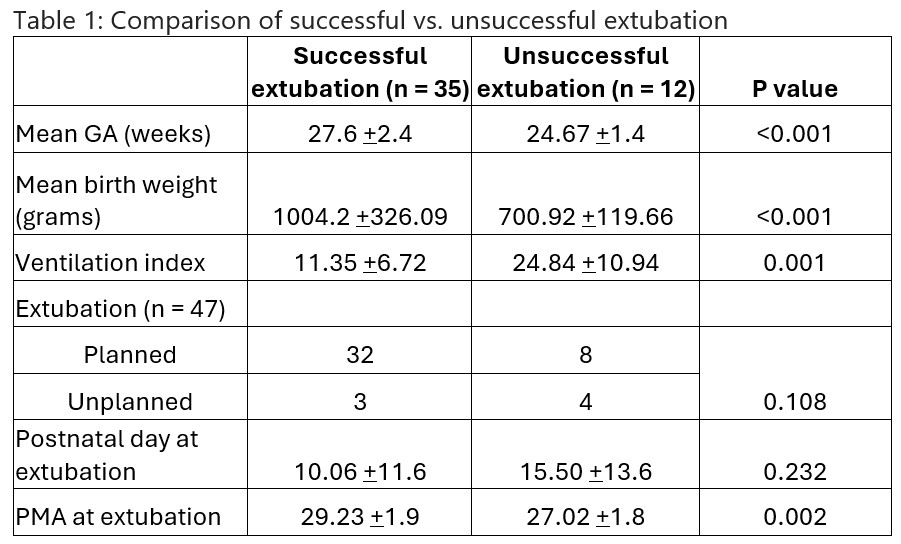
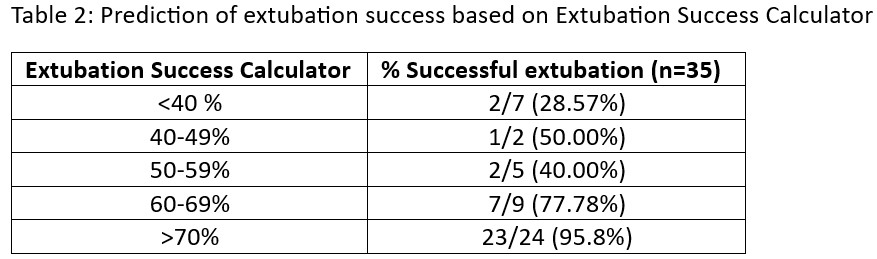
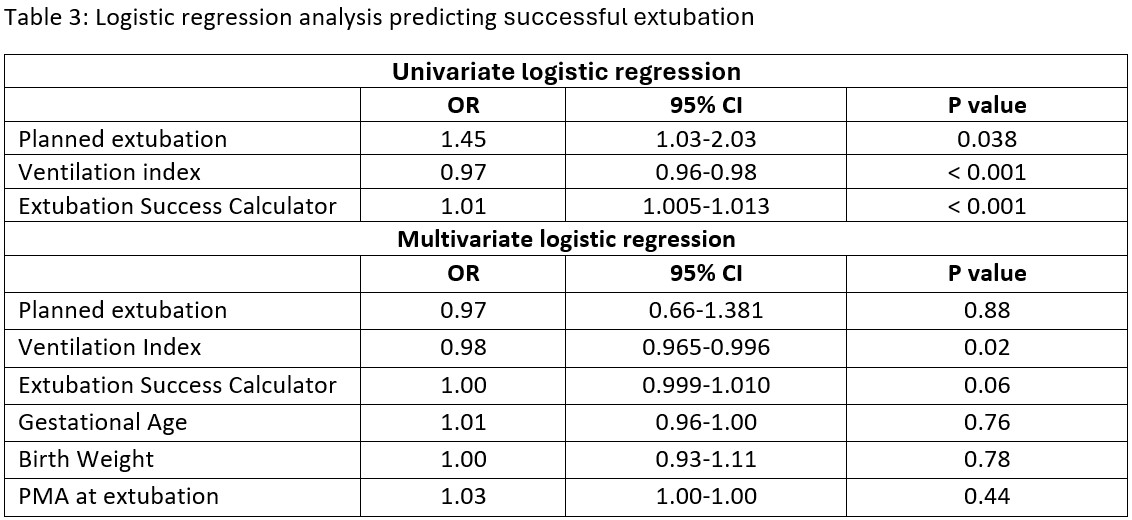
Results: A total of 37 infants were included with a mean GA of 27 ± 2.5 weeks and birth weight of 984 ± 328 grams. There were 47 extubation events, and 74% were successful. Unsuccessful extubation was significantly associated with a lower GA, birth weight, postmenstrual age (PMA) and higher VI (Table 1). An ExSC probability of >70% is associated with the best chance of successful extubation, and < 40% with the worst extubation outcome (Table 2). On unadjusted analysis, the odds of successful extubation were significantly correlated with planned extubation, VI, and ExSC (Table 3). On multiple regression analysis only VI remained significantly predictive of extubation success. The odds of successful extubation decreased at a rate of 0.98x for each increased point in the VI (95% CI 0.965-0.996, p=0.02)
Conclusion(s): In our patient population, an Extubation Success Calculator probability >70% is the best predictor of successful extubation. This study found that pre-extubation Ventilation index is a better predictor of successful extubation. We speculate that accurate prediction of successful extubation will require a combination of clinical and ventilation parameters and warrants further research.