Obesity
Session: Obesity 1
601 - Cardiometabolic Risk Attributable to Elevated BMI in Adolescence – A Propensity Score Analysis of Add Health Data
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 601
Publication Number: 601.2952
Publication Number: 601.2952

Dedeepya Konuthula, MD (she/her/hers)
Primary care research fellow
University of Chicago Division of the Biological Sciences The Pritzker School of Medicine
Chicago, Illinois, United States
Presenting Author(s)
Background: Many factors including social drivers of health influence both weight and cardiometabolic risk. Studies that have attributed elevated cardiometabolic risk to elevated body mass index (BMI) in adolescence using observational data have not sufficiently accounted for confounders.
Objective: To calculate a more accurate estimate of the risk of metabolic syndrome at 20 year follow-up due to elevated BMI in adolescence by balancing sociodemographic covariates (observable confounders) between groups.
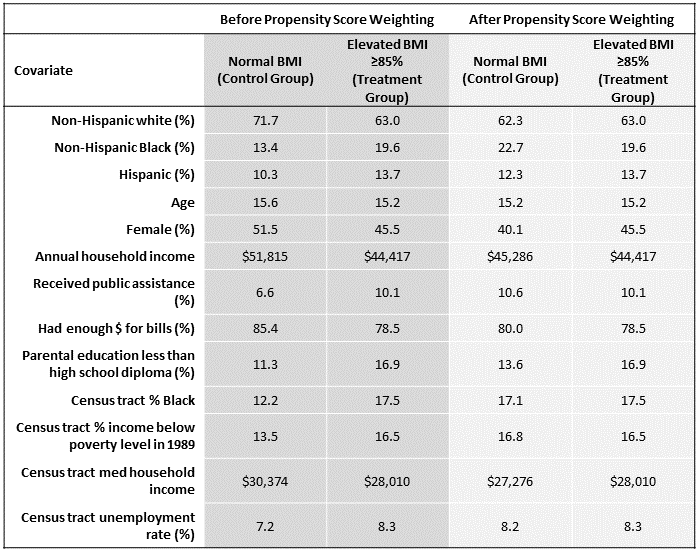
Design/Methods: The study cohort includes National Longitudinal Study of Adolescent to Adult Health (Add Health) participants who had both wave I data in 1994-1995 while in grades 7-12 and wave V biomarker results at 20 year follow-up in 2016-2018 (n=4,412). The adolescent cohort was divided into two groups: normal BMI ( < 85th BMI percentile for age and sex) and elevated BMI meeting criteria for overweight or obesity (≥85th%). Propensity score (PS) weighting is a causal inference method that weights participants based on PS (estimated probability of exposure given covariates) to balance observed confounders between groups. We used multiple imputation to impute missing parental socioeconomic variables (missing=14%) before PS weighting was used to balance covariates including race, parental socioeconomic status, and census tract level neighborhood data between the normal and elevated BMI groups. The outcome of interest was whether participants met diagnostic criteria for metabolic syndrome based on waist circumference, blood pressure, insulin resistance, and lipid measurements after 20 years.
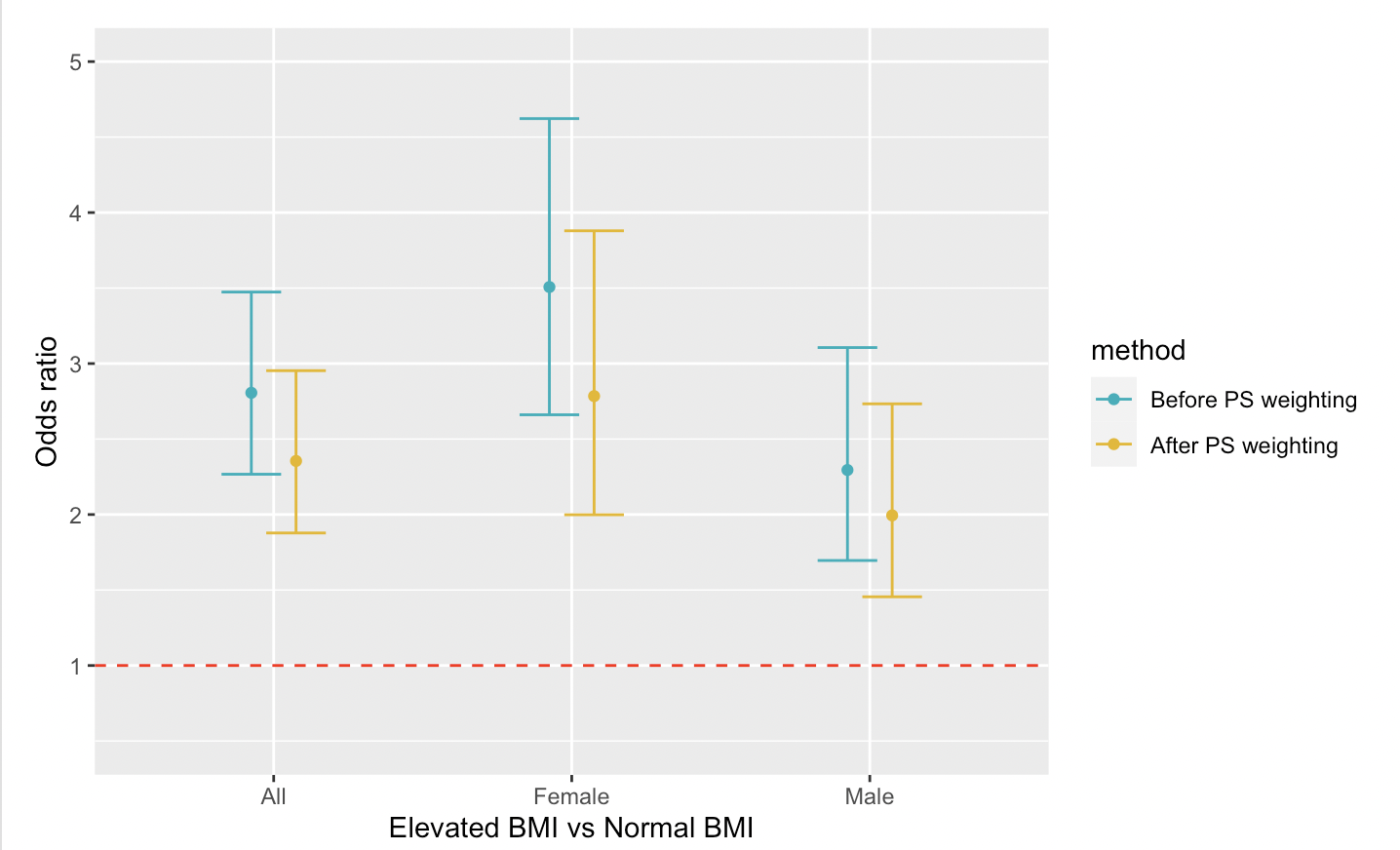
Results: After PS weighting improved the covariate balance between the groups (Table 1), being in an elevated BMI group in adolescence increased the odds of metabolic syndrome diagnosis at 20 year follow-up (OR 2.35, 95% CI 1.88-2.95). This relationship (Figure 1) is decreased when compared to traditional logistic regression before PS weighting (OR 2.81, 95% CI 2.27-3.47) and varies by sex (increased in women).
Conclusion(s): Elevated adolescent BMI is associated with metabolic syndrome at 20 years, though the association is weaker after accounting for observed confounders in a balanced analytic sample. Some of the cardiometabolic risk previously attributed to elevated BMI may be due to the complex effects of historical and ongoing structural racism and poverty. Thus, we need to prioritize structural solutions to advance equity and facilitate health-promoting behaviors in addition to the ever increasing focus on decreasing weight and BMI in adolescents through interventions like anti-obesity medications and bariatric surgery.