Neonatology
Session: Neonatal General 5: PDA, Surgical Conditions, Infections
143 - A Pilot Study to Examine the Association Between Intestinal Microbiome and Patent Ductus Arteriosus in Preterm Infants
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 143
Publication Number: 143.2100
Publication Number: 143.2100

Teahyen Cha, MD-PhD (he/him/his)
Clinical Professor
Gangnam Severance Hospital
Seoul, Seoul-t'ukpyolsi, Republic of Korea
Presenting Author(s)
Background: Numerous studies have shown a strong association between the intestinal microbiota and heart failure. Even if transient, hemodynamically significant Patent Ductus Arteriosus (hs-PDA) in preterm infants can manifest as symptoms of heart failure, coinciding with a period of rapid changes in the intestinal microbiota. Nonetheless, to date, no study has examined the correlation between the intestinal microbiome and preterm infants presenting heart failure symptoms due to hs-PDA.
Objective: The primary aim of this pilot study is to elucidate potential correlations between preterm infants with hs-PDA and their intestinal microbiome.
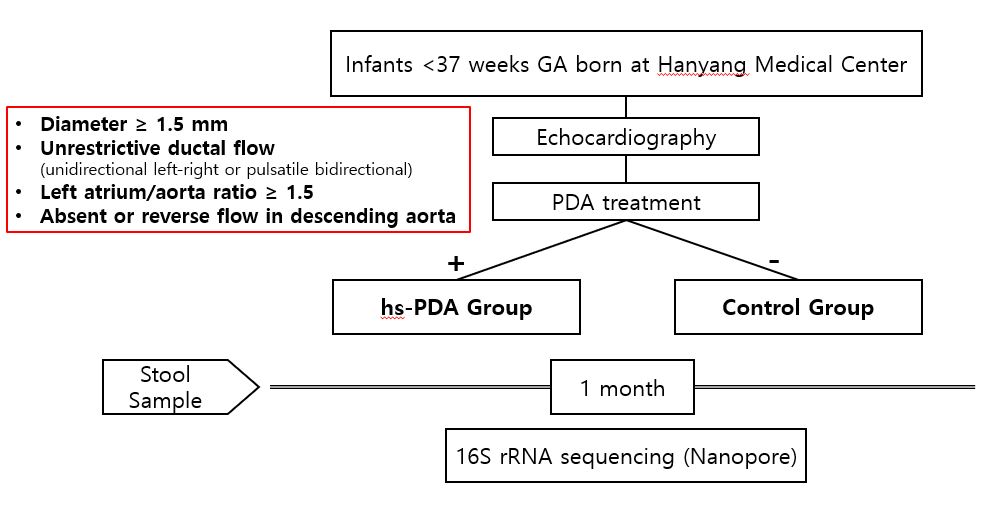
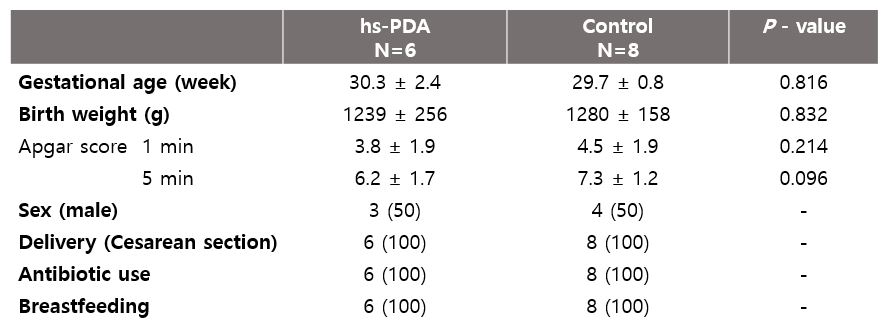
Design/Methods: This study enrolled six preterm infants with hs-PDA who were admitted to Hanyang University Hospital from September 2021 to December 2021. A total of eight preterm infants without hs-PDA and matched for gestational age, sex, weight, delivery mode, and use of antibiotics were selected as control group. Fecal samples were collected at one month after birth and subjected to 16S rRNA gene sequencing using Nanopore.
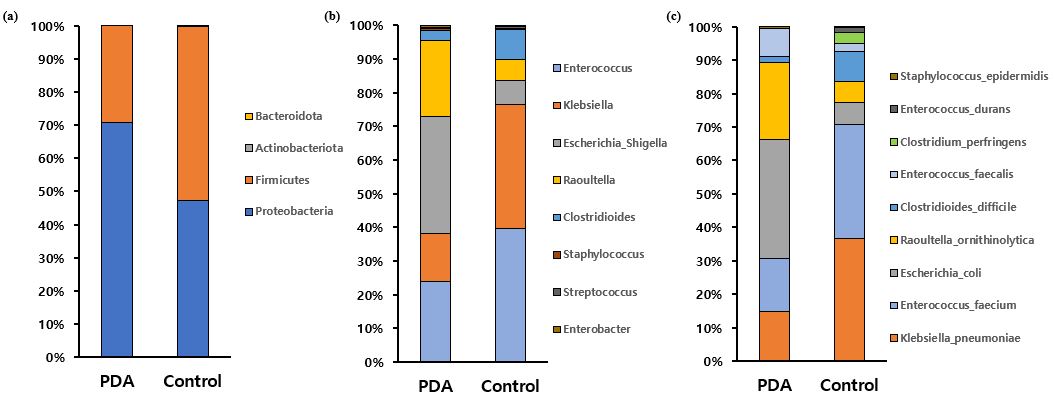
Results: The intestinal microbiome composition was significantly disordered in preterm infants with the hs-PDA group compared to the control group. At the phylum level, the hs-PDA group was predominantly composed of Proteobacteria and Firmicutes, whereas Proteobacteria in the control group was almost comparable to Firmicutes. In spite of the same Proteobacteria phylum, distinct differences in bacterial compositions were observed at the genus level between the two groups. The dominant genera identified in the hs-PDA group were Escherichia_Shigella, followed by Raoultella, and Klebsiella. In the control group, the dominant genus was Klebsiella, followed by Escherichia_Shigella, and Raoultella. At the species level, the hs-PDA group showed a higher abundance of E. coli and R. ornithinolytica, and E. faecalis whereas the control group had higher abundance of K. pneumoniae and E. faecium, and C. perfringers. The α-diversity was slightly higher in the control group than the hs-PDA group, although the differences were not statistically significant. Furthermore, the β-diversity showed no significant differences.
Conclusion(s): hs-PDA in preterm infants may cause intestinal microbiome dysbiosis, characterized by an increase in pathogenic bacteria and a decrease in beneficial bacteria. Additionally, hs-PDA in preterm infants showed a decreased tendency in α-diversity. Further study of the underlying mechanism is needed in large cohorts.