Neonatology
Session: Neonatal Fetal Nutrition & Metabolism 2: Fetal/Neonatal Metabolic Dyscrasias
129 - Associations between Maternal Glycemia and Infant Adiposity with Neonatal Interstitial Blood Glucose.
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 129
Publication Number: 129.346
Publication Number: 129.346

Rana Abdel-Rahman, MPH (she/her/hers)
Clinical Research Coordinator II
Brigham and Women's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Current neonatal hypoglycemia (NH) screening guidelines monitor infants of mothers with diabetes, but variability in diabetes phenotype and subsequent impact on NH outcomes has not been studied. Optimizing NH risk stratification algorithms requires a nuanced understanding of maternal and infant factors on the pathway to NH.
Objective: Examine the role of maternal and infant characteristics associated with neonatal interstitial blood glucose (IBG) patterns and odds of NH in the first 24 hours of life.
Design/Methods: This preliminary analysis included 17 mother-infant dyads enrolled in the ongoing LAMMBS (Late Antenatal Maternal Metabolism and Babies’ Sugar) prospective cohort study in Boston, MA. After delivery, we monitored infants’ IBG with blinded continuous glucose monitors (CGM). We measured neonatal adiposity using air displacement plethysmography within 72 hours of life. Early prenatal body mass index (BMI), glucose loading test (GLT) and glucose tolerance test (GTT) values were abstracted from maternal medical records. BMI was categorized by WHO and glycemia values were categorized per Carpenter-Coustan criteria: normal glucose tolerance (NGT: GLT < 130 mg/dL), gestational glucose intolerance (GGI: GLT ≥130 but < 190 mg/dL and 0 or 1 abnormal GTT values), and gestational diabetes mellitus (GDM: GLT ≥190 or GLT ≥130 but < 190 mg/dL and 2+ abnormal GTT values). Mothers with pre-existing Type 2 diabetes (T2D) were categorized separately. NH was defined as an IBG value < 45 mg/dL for ≥10 consecutive minutes. We used linear and logistic regressions, adjusting for CGM placement duration, to examine associations between exposures with IBG patterns and the odds of any NH event. We used STATA’s sem command to assess causal mediation.
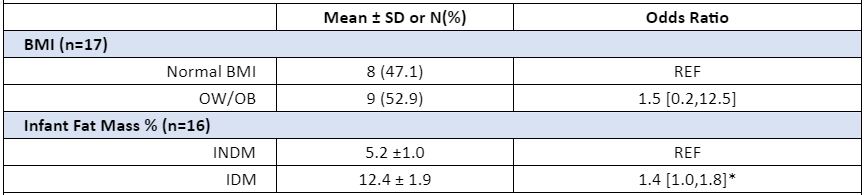
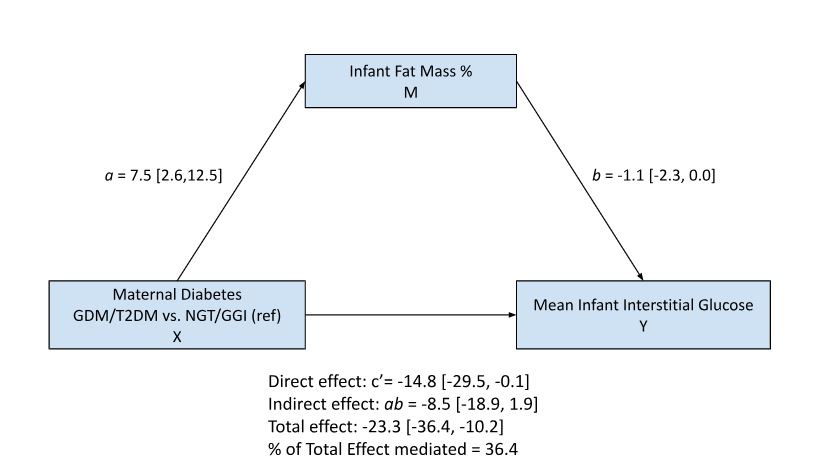
Results: Eleven (65%) mothers in our cohort had diabetes, 5 (29%) of whom had GDM and 6 (35%) of whom had T2D. GDM (β-23.4 mg/dL; 95% CI -45.2, -1.6) and T2D (β-26.3 mg/dL; 95% CI -47.2,-5.3), but not GGI, were significantly associated with lower mean IBG values than NGT (Table 1). Mean infant fat mass % was associated with lower (β -1.8 mg/dL; 95% CI -3.1, -0.5) mean IBG values. Infants with higher fat mass % had higher odds (OR 1.4; 95% CI 1.0,1.8) of having an NH event (Table 2). Infant fat mass mediated 36% of the association between maternal diabetes and IBG (Figure 1). Maternal BMI was not significantly associated with NH.
Conclusion(s): Infant adiposity partially mediates the association between maternal glycemia and NH and may present an opportunity to improve NH risk stratification criteria. Data collection is ongoing and results to be confirmed in the full cohort.
.jpg)