Neonatology
Session: Neonatal Neurology 5: Clinical
542 - Using Cord Blood Proteomics to Identify Predictive Markers of Intraventricular Hemorrhage in Preterm Infants
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 542
Publication Number: 542.1352
Publication Number: 542.1352

Priyanka Ramanan (she/her/hers)
Medical Student
Northwestern University The Feinberg School of Medicine
Chicago, Illinois, United States
Presenting Author(s)
Background: Preterm birth is associated with comorbidities, including intraventricular hemorrhage (IVH), a clinically silent syndrome in which clinical examination fails to detect signs of a lesion in up to 50% of cases. The presence of IVH is associated with future neurodevelopmental impairment. Cord blood protein biomarkers may provide valuable information about the prenatal environment and have been associated with other neonatal conditions such as early-onset sepsis. In previous literature, serum biomarkers S-100 β and activin A were found to be associated with IVH, although none are utilized clinically currently.
Objective: To determine cord blood protein markers associated with IVH and if these markers, individually or in combination, can predict the incidence and/or severity of IVH.
Design/Methods: Archived cord blood samples (n=223 total, n=121 < 33 weeks GA) underwent untargeted mass spectrometry proteomics (600ng/sample) in technical duplicates. Proteins were identified using the MaxQuant database search, and values were batch normalized. Data on neonatal clinical course, risk factors for IVH, medications, comorbidities, and IVH severity were collected through medical record review. Results of routine cranial ultrasounds for participants were reviewed. Computational modeling and statistical analysis included the Mann-Whitney U-test with Benjamini-Hochberg correction to determine proteins that differed significantly infants with IVH vs. no IVH (FDR-adjusted p-value < 0.05).
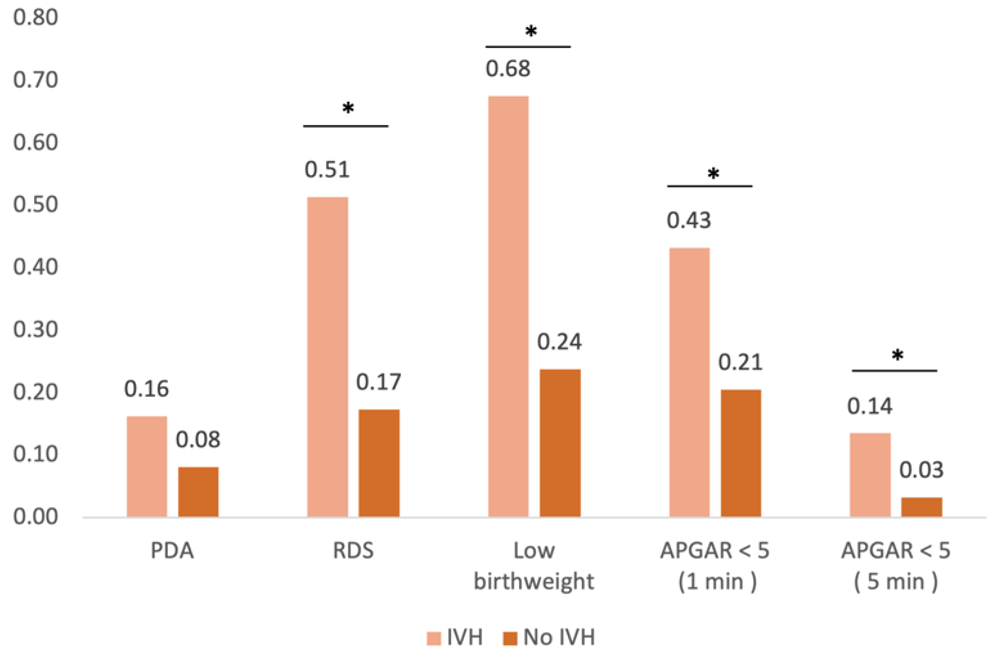
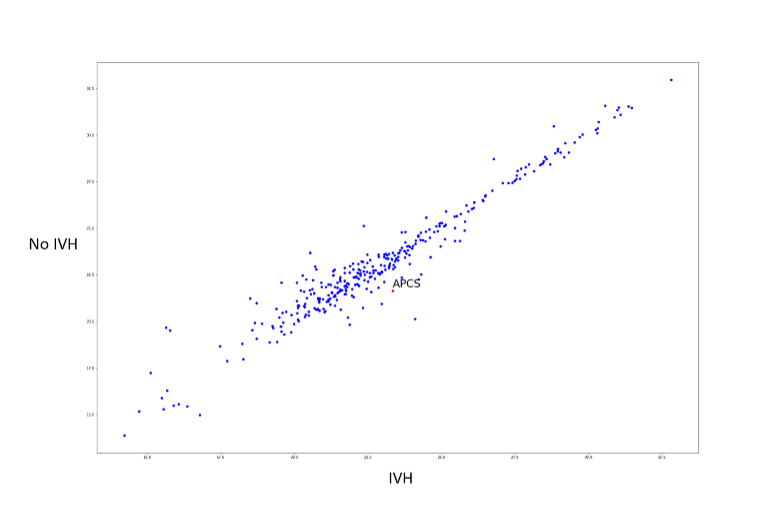
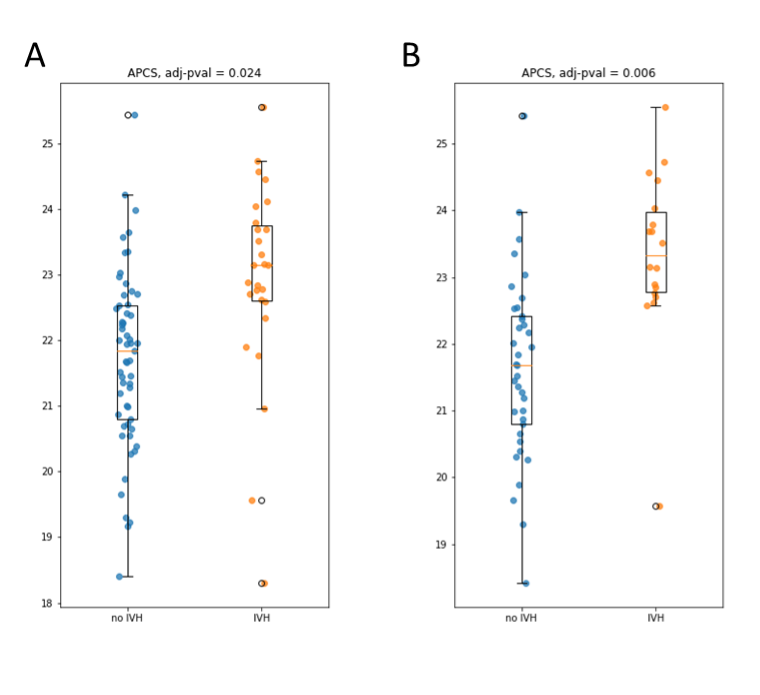
Results: The incidence of IVH among preterm infants was 31% (n=37/121); grade I IVH was most frequent (70%, n=26/121). Previously reported risk factors for IVH hold true in this cohort [Fig 1], including low birth weight, comorbid respiratory distress syndrome (RDS), and low APGAR scores. Serum amyloid P component (APCS) was significantly elevated in infants who developed IVH compared to those without IVH, both 1) in pooled analysis of infants 24-32 weeks GA (p=0.024) and 2) in stratified analysis by gestational age (GA) subgroup (29-32 weeks GA, p=0.006) [Fig. 2, 3]. C-reactive protein (CRP) levels were also elevated in the IVH group, though not statistically significant (adj. p=0.28)
Conclusion(s): Our findings suggest APCS, a suggested marker of tissue damage and immune response, as a potential cord blood protein to predict IVH in preterm infants < 33 weeks GA. A larger study cohort is required to further validate APCS and demonstrate potential significance for other markers like CRP. Cord blood markers may serve as a future strategy for rapid IVH risk stratification at birth to guide imaging and close neurodevelopmental follow-up.