Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 1
359 - Improving Our Shared Mental Model: A Trainee Led Intervention to Improve High Quality Discharges via Documentation of the Expected Discharge Date
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 359
Publication Number: 359.1886
Publication Number: 359.1886

Elizabeth C. Kuhn, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: In 2022, the inpatient census was persistently above capacity at a freestanding children’s hospital resulting in prolonged admission wait times and postponement of elective procedures. Prior work identified approximately one-fourth of patients at a tertiary care pediatric hospital may have been discharged earlier with delays attributed to poor discharge planning and miscommunication between team members. Tools to standardize interprofessional communication have resulted in decreased length of stay.
Objective: As part of an enterprise-wide multi-step quality improvement (QI) effort, a trainee-led team aimed to increase expected discharge date (EDD) documentation on resident teams with low utilization from 26% to 75% for all discharges by December 2023 via the EDD column, a standardized tool within the institution’s electronic health record (EHR).
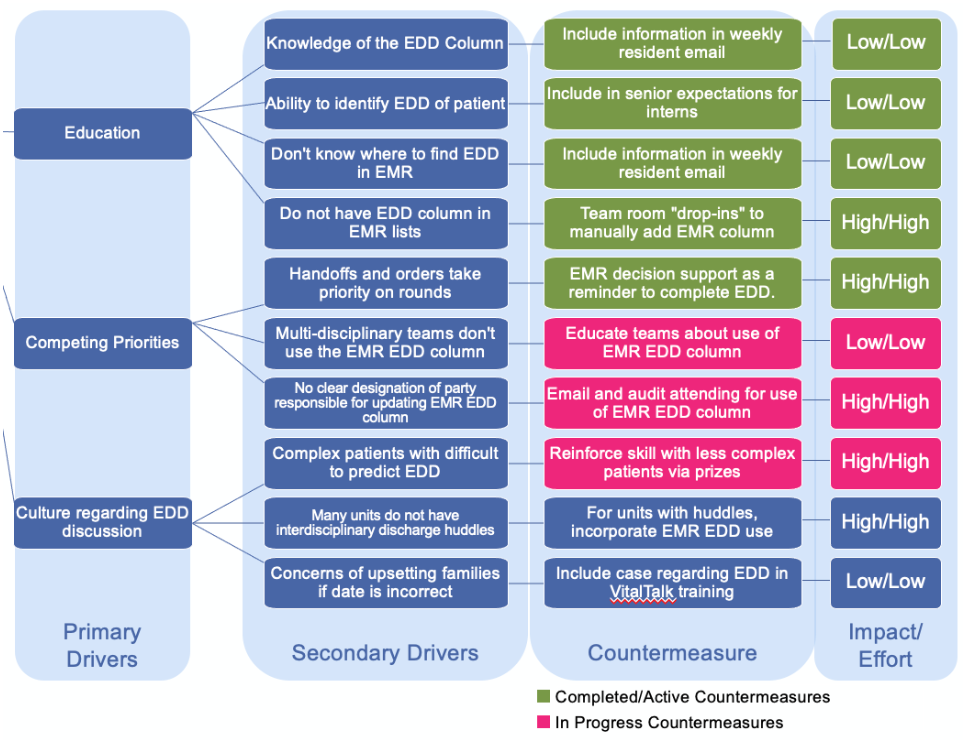
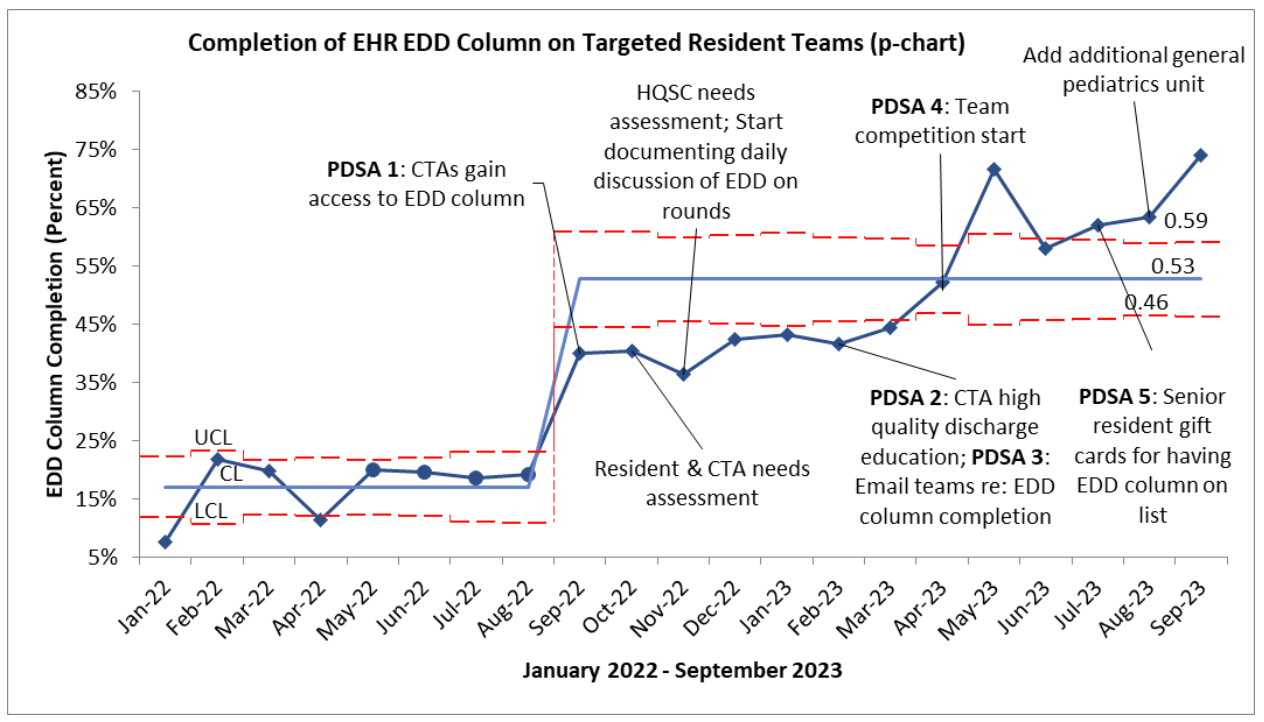
Design/Methods: Stakeholder mapping to identify barriers to EDD documentation informed the creation of a driver diagram. A needs assessment evaluated awareness and use of the EDD column, estimated EDD discussion frequency, and perceived benefit of the tool. Countermeasures were organized via an impact/effort matrix (Figure 1). Six units were identified for low EHR EDD documentation and targeted for intervention. Multiple PDSA cycles were conducted (Table 1). A monthly run chart monitored interventions and standard Associates in Process Improvement rules were applied (Figure 2). Measures included EHR EDD documentation (outcome), discussion of EDD on rounds (process), and length of rounds (balancing).
Results: 71% of resident respondents (n=68) reported the EDD column was a valuable tool and 13% used it. Baseline EDD documentation for target units was 26%. EDD documentation improved and demonstrated special cause variation resulting in a center line shift after PDSA 1 with a continued upward trend after PDSA 4 and 5. There was no special cause variation for EDD discussion on rounds or rounding time per patient.
Conclusion(s): Improved documentation of the EDD supports high quality discharges through a shared mental model between interdisciplinary team members. Our data demonstrated a sustained increase in EDD documentation following clinical decision support and educational interventions. Future interventions include audit/feedback and scheduled daily review with charge nurses. With improvement in EDD documentation, our current outcome measure will serve as a process measure in future QI work to examine high quality discharge outcomes such as length of stay, discharge medication delivery, restocked and/or wasted medication, and follow-up appointments scheduled.
.png)
