Emergency Medicine
Session: Emergency Medicine 5: Sepsis
126 - Infections Encountered At A Pediatric Emergency Department When Sepsis Alert Criteria Is Triggered
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 126
Publication Number: 126.1524
Publication Number: 126.1524
- GT
Godfrey Tutay, MD
Attending Physician - Pediatric emergency medicine
NYU Langone Hospital Long Island, Department of Emergency Medicine
east meadow, New York, United States
Presenting Author(s)
Background: Sepsis is an infection induced response that can cause multi-organ system failure. Early detection and recognition are vital in alleviating morbidity and mortality. At our hospital, a screening tool in the emergency department (ED) including fever/low temperature with any heart rate or respiratory abnormality or a low blood pressure, all age specific, triggers a notification for a bedside huddle with a physician.
Objective: This study aimed to investigate the performance of our screening tool based on the type of infections encountered when it is triggered and whether it is effective in differentiating severe sepsis from uncomplicated pediatric infections.
Design/Methods: In this retrospective chart review, data was analyzed between Dec 1, 2021 and November 30, 2022 for children ages of 6 weeks to 19 years who triggered sepsis alert and patients who had a final diagnosis of sepsis prior to discharge, even if they did not trigger sepsis.
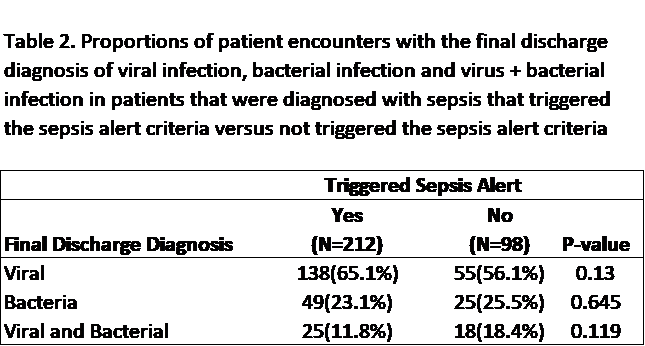
Results: There were 18,032 pediatric visits at our pediatric emergency department during the allotted period. Sixty-five patients were excluded. During that time 2,922 patients triggered sepsis alert, 212 (7.3%) of which were determined to have sepsis. Of these 212 patients; 138 (65%) were from viral infections, 49 (23%) from a bacterial etiology, and 25 (12%) from both bacterial and viral co-infections (Table 2). Furthermore, only 5 were determined to have severe sepsis with 3 of these being viral in origin. There were 2 patients found to have severe sepsis that did not trigger the sepsis criteria. 92.7% of patients that triggered sepsis did not have sepsis. There was no significant difference in patients diagnosed with sepsis between patient that triggered the sepsis alert and those that did not (Table 1). The positive predictive value of the screening tool for sepsis and severe sepsis/sepsis shock were 8.3% and 0.2%, respectively (Figure 1 and 2).
Conclusion(s): This retrospective chart review concludes that the sepsis alert criteria over triggers and many of the triggers are due to viral infections. Furthermore, our data showed that the screening tool is not a good predictor of sepsis as it fails to reach significant difference from patients that did not trigger sepsis alert.
.png)