Developmental and Behavioral Pediatrics
Session: Developmental and Behavioral Pediatrics 2: Autism
404 - Autism, Vaccines, and Trust: Do lower levels of trust in physician-provided vaccine information impact COVID-19 vaccine decisions by parents and families with autistic children?
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 404
Publication Number: 404.266
Publication Number: 404.266
Lauren B. Stumpp (she/her/hers)
Medical Student
University of Pittsburgh School of Medicine
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Background: Vaccine-preventable illnesses have surged in recent decades as immunization rates have fallen, leading to unnecessary pediatric hospitalizations and deaths. Parents and families with autistic children (PFAC) have historically reported high rates of vaccine hesitancy. Despite numerous studies refuting an association, PFAC have cited concerns that childhood vaccines contributed to or caused their child’s autism. A trusting relationship with their child’s physician is linked with improved rates of vaccine acceptance amongst the general pediatric population; however, the role of physician trust has not been specifically explored amongst PFAC as a factor to lessen vaccine hesitancy in this high-risk group. In this study, we explore whether the perceived level of physician trust amongst PFAC is associated with higher vaccination rates, and specifically the COVID-19 vaccination series.
Objective: To characterize the influence of physician trust on COVID-19 vaccine decisions amongst PFAC.
Design/Methods: PFAC (children age range 18mo-17y) were recruited through the University of Pittsburgh voluntary research collective “Pitt+Me” (https://pittplusme.org/) to complete an online survey about their child’s vaccination status, experience during COVID-19, and relationship with their child’s physician, including questions adapted from the Trust in Physician scale developed and validated by Hall, et. al. in 2001. Statistically significant differences between groups were calculated using Fisher’s exact tests, chi-square analyses, and ANOVAs as indicated, and Mann-Whitney non-parametric tests for trust scale questions.
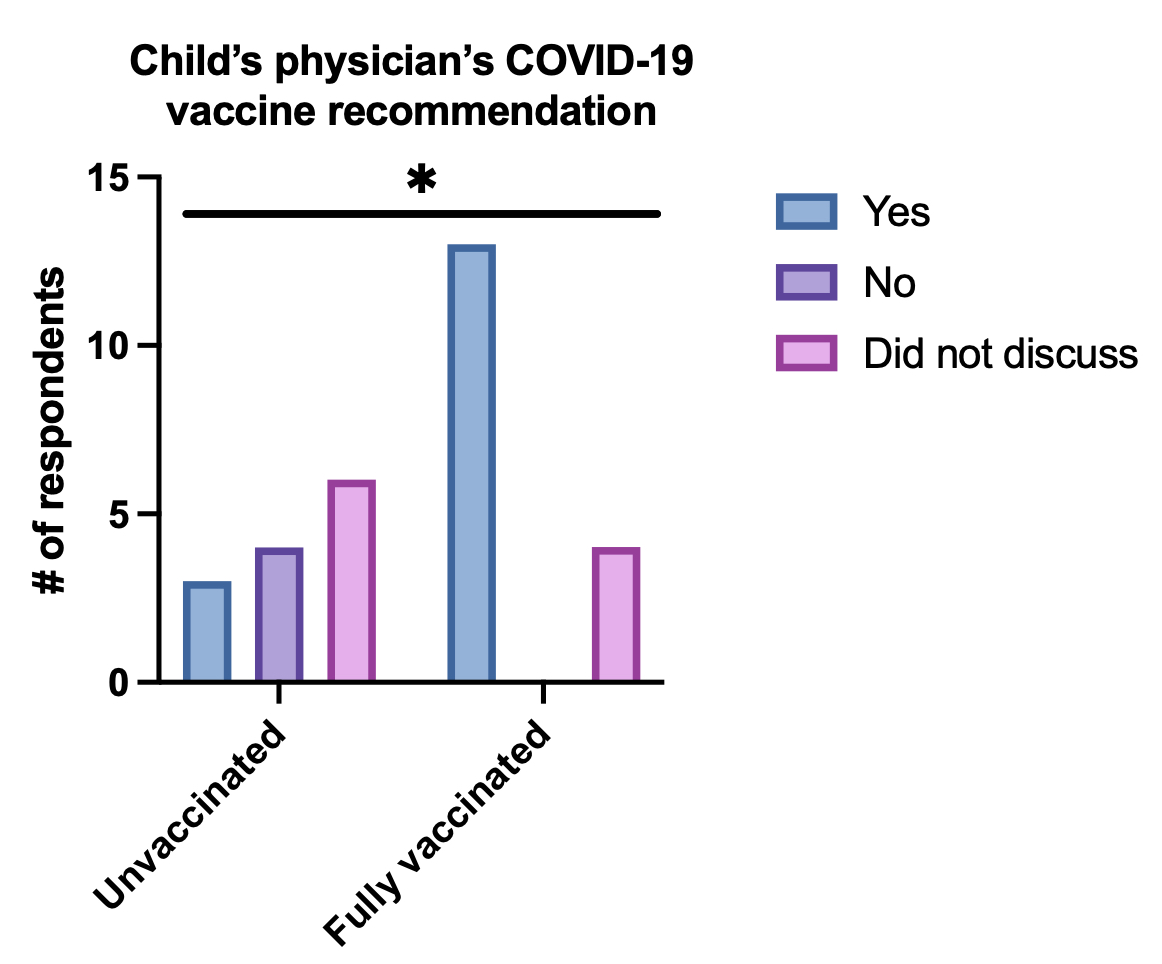
Results: For autistic children who were not vaccinated against COVID-19, PFAC were younger, attained lower degrees of education, lived in rural/suburban communities at higher rates, and had children diagnosed with autism at older ages. In the unvaccinated group, PFAC were also more likely to report their child’s doctor recommended against or did not discuss the COVID-19 vaccine. PFAC in the unvaccinated group did not report a significant deficiency in trust when asked about general trust in their child’s physician, but they did score significantly lower in 6 out of 11 trust questions specific to information about vaccines and COVID-19.
Conclusion(s): PFAC who did not vaccinate their children for COVID-19 endorsed less trust in the physician-provided information on vaccines and COVID-19 and were less likely to have received recommendations to vaccinate by their child’s physician.
.jpg)
.jpg)
