Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 9
332 - Is parental language selection associated with neurodevelopmental outcomes among infants with acute provoked neonatal seizures in the USA?
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 332
Publication Number: 332.1904
Publication Number: 332.1904

GRETA S. PENG, MD (she/her/hers)
Child Neurology Resident
UCSF Benioff Children's Hospital San Francisco
San Francisco, California, United States
Presenting Author(s)
Background: Parental non-English language preference (NELP) is associated with worse pediatric health outcomes in the USA. Infants with acute provoked neonatal seizures (APNS) may require longitudinal health care access and follow up that puts patients with parental NELP at risk for poorer outcomes. Little is known about the association between parental NELP and neurodevelopmental outcome specifically in infants with APNS.
Objective: To evaluate the relationship between parental NELP and neurodevelopmental outcome in a multi-center cohort of infants with APNS.
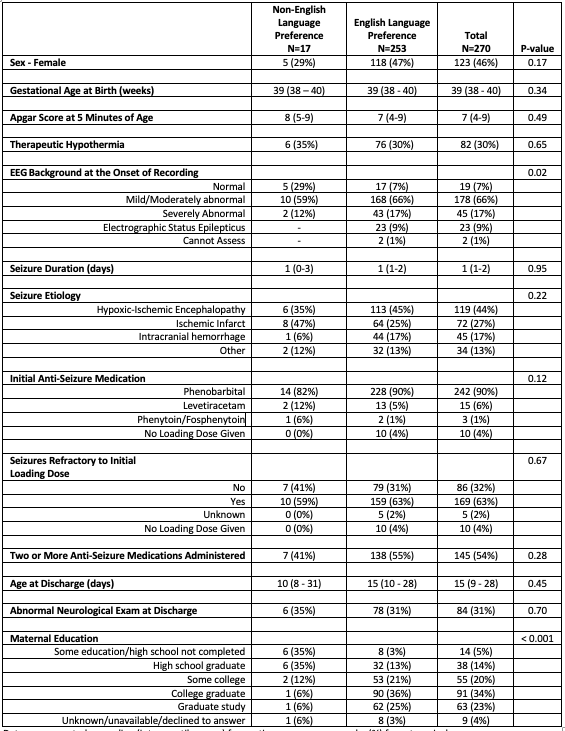
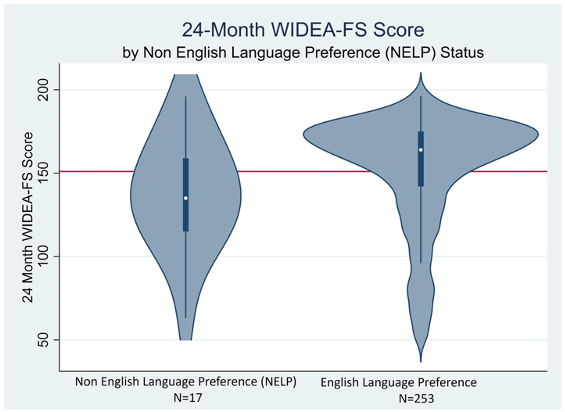
Design/Methods: Infants in the Neonatal Seizure Registry-II were included. Parental NELP was present if a medical interpreter was used for research consent. The Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA-FS) score was conducted by a research coordinator in the parents’ preferred language at age 24 months. Multivariate regression was used to examine the association between NELP and WIDEA-FS. Functional developmental impairment (FDI) was defined as two standard deviations (SD) below the mean. Multivariate models were refined by removing non-significant covariates from the full model in a backwards stepwise fashion until covariates were significant contributors to the model.
Results: Among 270 children with APNS, 17(6%) had parents with a Spanish language preference (NELP). There were no significant differences between groups for key clinical co-variates (Table) except for maternal education and EEG background. After adjusting for EEG, hypothermia treatment, seizure etiology, and age and neurological exam at discharge, infants with parental NELP had a WIDEA score that was on average 10 points (1 SD) lower when compared to infants without parental NELP (95% CI -24 to 3,p=0.13,Figure) and more than five times the odds of FDI (OR 5.4,95% CI 1.6-17.9,p=0.007). Maternal education was not significant in the multivariate model.
Conclusion(s): Infants with APNS with parental NELP were more likely to have functional impairment at 24 months when compared to infants without parental NELP. This is consistent with studies showing the association between parental NELP and worse health outcomes. To fully understand these results, we must recognize that parental NELP is likely a proxy for discriminatory experiences which impact health and socioeconomic opportunities, and not a biological construct. Future studies must examine the root causes of neurodevelopmental differences and create interventions to address them. Limitations include the small number of infants with parental NELP and the absence of cross-cultural validity of the WIDEA-FS.