Hematology/Oncology
Session: Hematology/Oncology
352 - Increased Sepsis Attributable Mortality in Pediatric Hematology Oncology and Transplant Patients is Associated with Lack of an Early Recognition Tool
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 352
Publication Number: 352.228
Publication Number: 352.228

Hana Hakim, MD, MS
Full Member, Department of Infectious Diseases; Medical Director, Infection Prevention and Control
St. Jude Children's Research Hospital
Memphis, Tennessee, United States
Presenting Author(s)
Background: Sepsis is a common complication in pediatric hematology/oncology and transplant (PHOT) patients and is associated with significant morbidity and mortality. Quality improvement (QI) initiatives have focused on earlier recognition and intervention for sepsis in the emergency department (ED), but QI focusing on hospital-onset sepsis (HOS) among inpatient immunocompromised children remains lagging.
Objective: To characterize PHOT patients who develop HOS in inpatient care settings and identify risk factors for 30-day sepsis-attributable (SA) mortality.
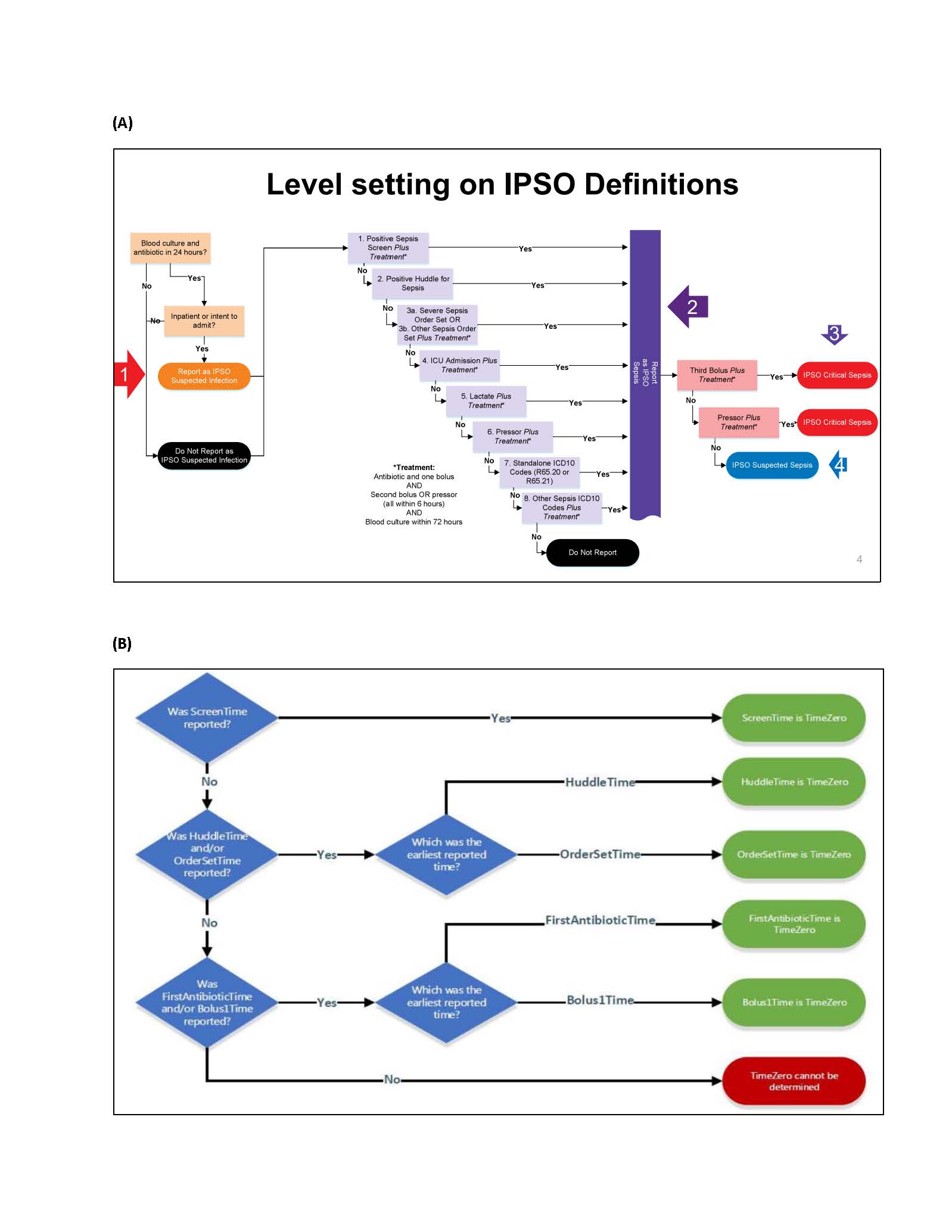
Design/Methods: We analyzed an existing dataset of sepsis in PHOT patients prospectively collected over five years (2017-2021) as part of a multicenter QI initiative, the Improving Pediatric Sepsis Outcomes (IPSO) Collaborative. Figure 1A shows IPSO operational definition for identification of patients with sepsis and Figure 1B IPSO operational definition for determination of functional time zero (FTZ) of sepsis onset. HOS was defined as episodes with FTZ of >12 hours after admission time to the hospital. Multivariable generalized linear mixed modeling, assuming a binomial distribution and logit link, assessed factors associated with 30-day SA mortality.
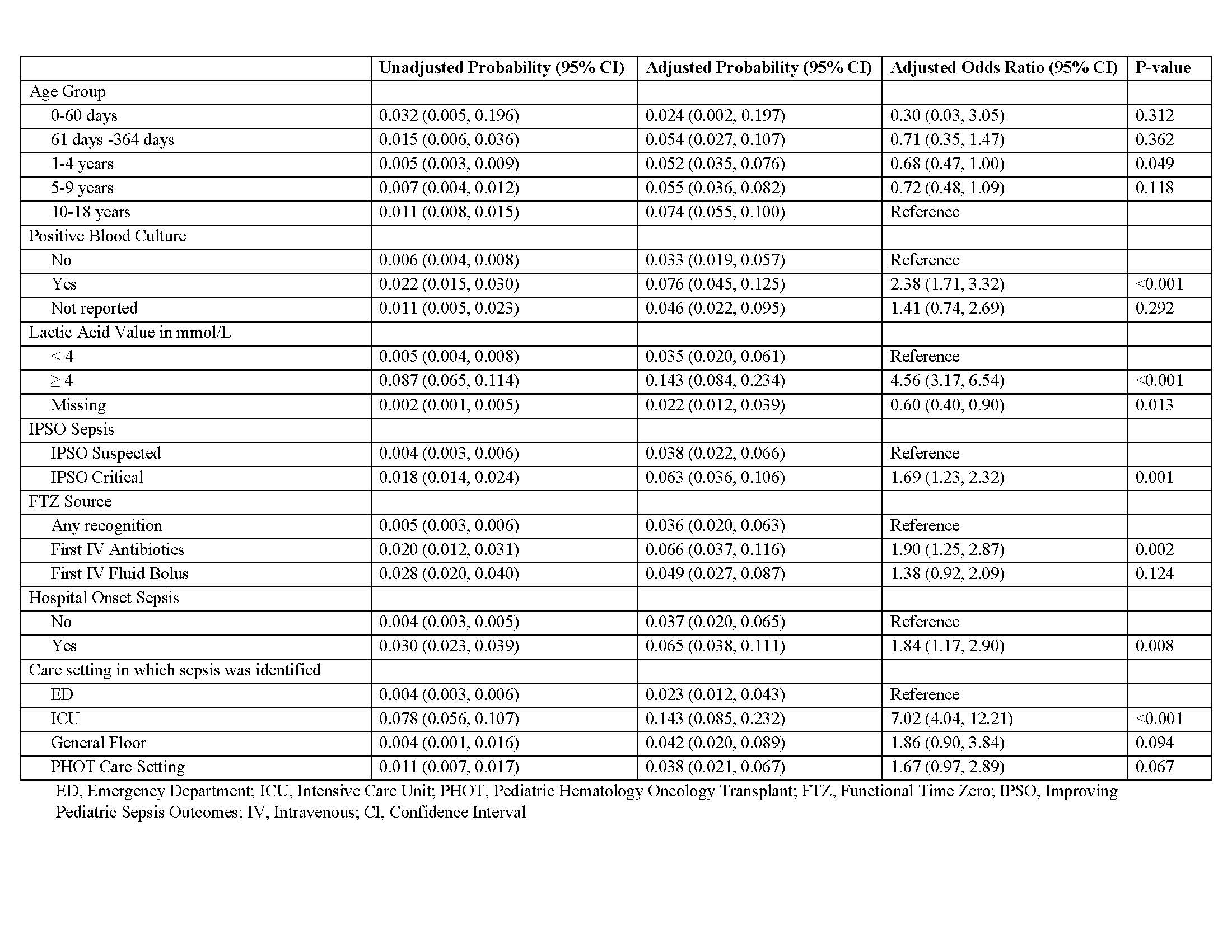
Results: A total of 9,604 sepsis episodes in PHOT patients from 49 hospitals were distributed as follows: 70.5% presented to ED, 10.9% developed within the first 12 hours from admission, and 18.6% were HOS. Most (87.2 %) PHOT patients presenting to the ED were identified using a sepsis recognition method compared to 52.5% with HOS (p < 0.001). The 30-day SA mortality in the overall cohort was 2.2% with a significantly higher rate (6.9%) among those with HOS versus those who developed sepsis at presentation or in the first 12 hours (1.1%, p< 0.001). The table shows independent risk factors for 30-day SA mortality among PHOT patients. Compared with those identified by a sepsis recognition method, PHOT patients identified as having sepsis by IV antibiotics were more likely to die from sepsis in both the HOS cohort [adjusted OR 2.11 (95% CI, 1.14-3.92)] and the non-HOS cohort [adjusted OR 2.74 (95% CI, 1.47-5.10)] (Figure 2).
Conclusion(s): PHOT patients with sepsis were better recognized in ED care settings using a recognition method than in inpatient care settings. The 30-day SA mortality was lower in inpatient settings when sepsis was detected by early recognition methods, supporting the need for stronger QI efforts to implement sepsis recognition tools more broadly in the PHOT inpatient setting.
.jpg)
