Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 2
373 - A Pediatric and Adolescent High-Risk Behavioral Health Ambulatory Safety Net
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 373
Publication Number: 373.1968
Publication Number: 373.1968
.jpg)
Joanne E. Cox, MD (she/her/hers)
Associate Chief, Division of General Pediatrics
Harvard Medical School
Boston, Massachusetts, United States
Presenting Author(s)
Background: Pediatric behavioral health (BH) concerns present safety and quality risks due to failure to identify and characterize problems, or to connect patients to BH services. Failed closure of communication loops is a major barrier. Ambulatory Safety Nets (ASN) create highly reliable systems to prevent diagnosis or care delays and are used for adult cancer screening and depression. ASNs have not been previously studied in pediatric BH. This work was part of a learning collaborative organized by CRICO/Risk Management Foundation and Ariadne Labs.
Objective: Our objective was to improve population management and care coordination by implementing a novel ASN focused on connection to care for patients with highest risk BH diagnoses at two pediatric practices in Boston, MA.
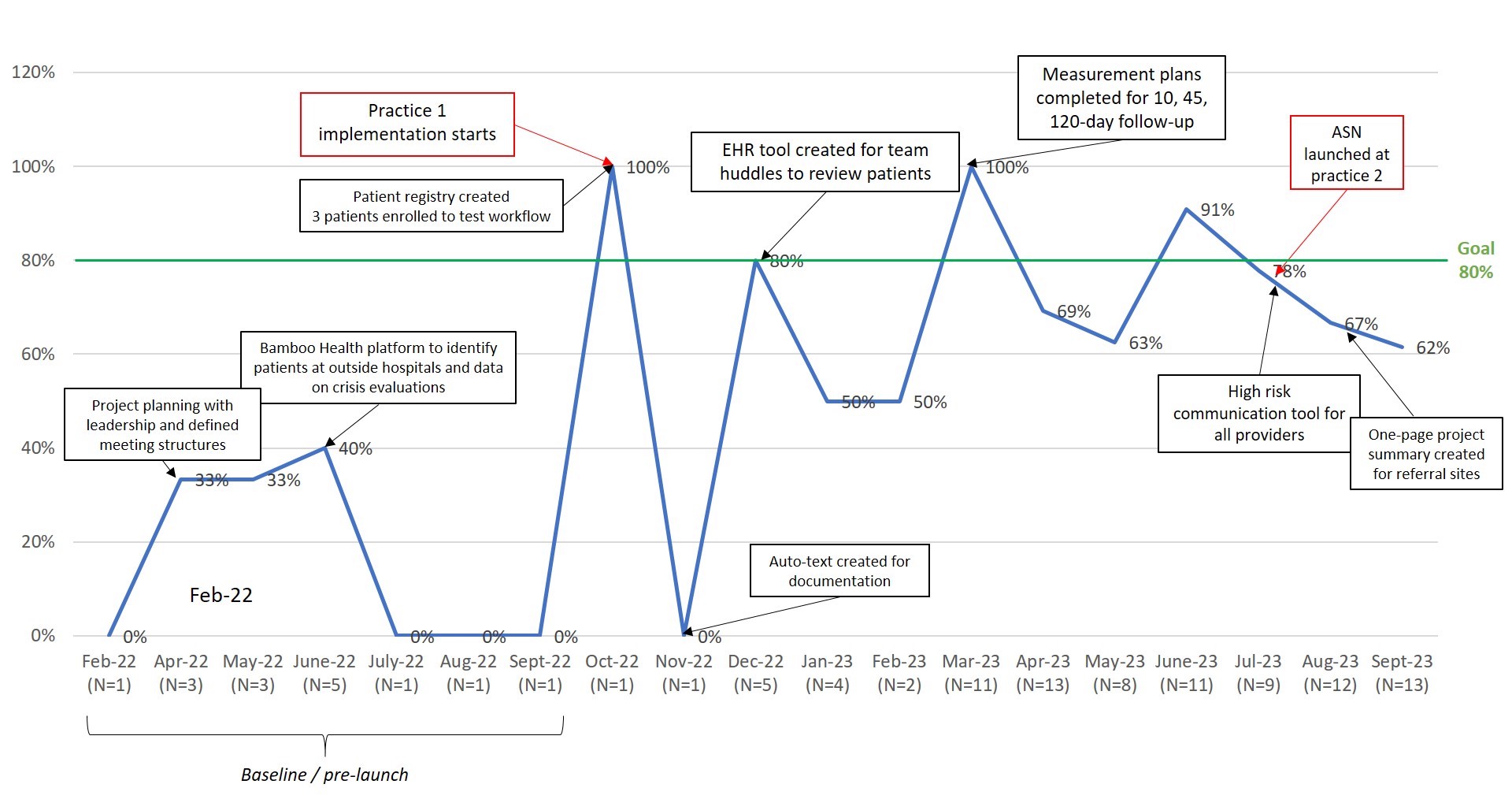
Design/Methods: The project began at practice 1 (6,000 empaneled patients) in October 2022 and expanded to practice 2 (16,000 patients) in July 2023. A working group defined BH highest risk as hospitalization, boarding in an emergency department or awaiting higher level of care after community emergency assessment. The team created a driver diagram and process maps. Primary drivers were obtaining leadership support, establishing clinical standards, building registry and workflow redesign. Measures were BH care coordination follow-up at 10, 45 and 120 days and readmission rates. Annotated run charts were used to track early process. Qualitative team interviews identified challenges.
Results: 90 patients were enrolled through Sept 2023. Patients were 64% female; 48% Hispanic, 30% Black, non-Hispanic. Median age was 14 years (range 6-22 years). Implementation of the BH ASN increased our care coordination follow up within 10 days of discharge from 27% to 73% (Figure 1). Care coordination at 45 days maintained at 69% (Figure 2). Readmission rates within 45 days of discharge decreased from 16% to 7%. (Figure 3). Challenges were obtaining timely data on discharges, contacting patients as number of managed patients increased, and finding long-term therapy options.
Conclusion(s): The BH system is often fragmented. Our BH ASN enhanced management of high risk BH patients by creating a registry, improving accurate data flow and processes for care coordination. As more patients entered the ASN, the 45 day measure remained stable. Identifying long-term therapy remained a barrier. For next steps, we will include the 120 day measure as more patients reach that mark. We will track data using control charts starting in Nov 2023. We plan development of an emergency department visit measure. A third practice will be added in Jan 2024.
.jpg)
.jpg)
