Neonatology
Session: Neonatal GI Physiology & NEC 3: GI Physiology and Probiotics
541 - Bacteremia following gastrointestinal contrast studies in neonates
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 541
Publication Number: 541.2095
Publication Number: 541.2095
.jpg)
Kylee A. Andrew, BS (she/her/hers)
Medical Student
University of Illinois College of Medicine Peoria
Peoria, Illinois, United States
Presenting Author(s)
Background: Many neonates presenting with gastrointestinal concerns require contrast radiographic studies during their NICU stay. These studies, while necessary for an accurate diagnosis and treatment plan, have been associated with bacterial translocation. Many are performed for primary diagnostic purposes, other neonates with a history of bowel perforation may require these studies for surgical planning. The latter group may be premature, low birth weight, and with a prolonged history of total parenteral nutrition and invasive central lines, placing them at especially high risk of bacterial sepsis. Recommendations have been made for antibiotic prophylaxis for populations at high risk of endocarditis, however there are no such recommendations at this time for neonates. This warrants a further look into sub-populations of high-risk neonates and whether the incidence of bacteremia is significant enough to indicate prophylactic antibiotic treatment.
Objective: We hypothesize that there is a significant proportion of neonates who develop bacteremia within 2 days of a gastrointestinal contrast enema study.
Design/Methods: This is a retrospective cohort study looking at neonates born from January 1, 2011 to December 31, 2021 admitted to a level IV NICU who had a lower gastrointestinal contrast study during their NICU stay. The primary outcome was the incidence of bacteremia within 48 hours of the study, with additional data collected including reason for GI study, history of bowel disease, presence of central line, and antibiotics at time of study.
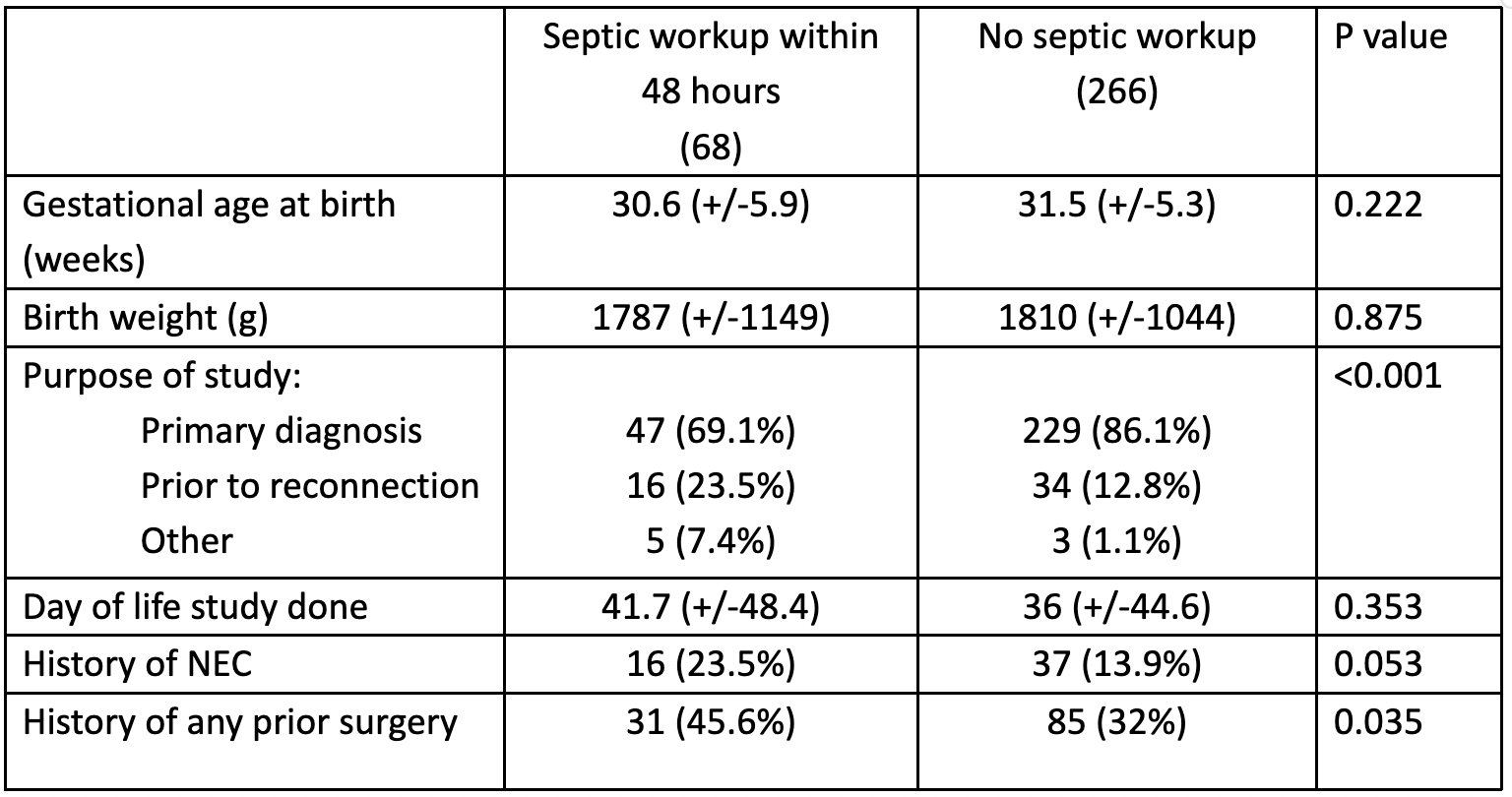
Results: The rate of bacteremia after a contrast study were low with 5 patients (1.5%) having a positive blood culture within 48 hours and 1 more between 48-72 hours of life. Those who did develop bacteremia were more likely to have a history of NEC and an ostomy, with the study occurring prior to reconnection at a later day of life. Antibiotic administration prior to the contrast study did not impact the rate of bacteremia or septic work-up. Patients commonly did experience a septic workup within 48 hours of the lower GI study, occurring after 20.4% of the lower GIs in this study.
Conclusion(s): While the rate of septic workups following GI studies was high, the rate of bacteremia was found to be low in this cohort. The few patients diagnosed with bacteremia had additional history which may better explain the sequelae than the lower GI study alone. These findings recommend against the use of prophylactic antibiotics in this population prior to a lower GI study. Further studies may examine the utility of prophylaxis specifically in neonates with ostomy prior to reconnection.
.png)