Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 5
39 - Targeting Inaccuracies in Linear Growth Measurements in the Neonatal Intensive Care Unit
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 39
Publication Number: 39.2809
Publication Number: 39.2809

Gail Snyder (she/her/hers)
Medical Student
McGovern Medical School at the University of Texas Health Science Center at Houston
Houston, Texas, United States
Presenting Author(s)
Background: Linear measurements are critical in the neonatal intensive care unit (NICU) for determining nutritional status of a newborn. Length is a marker of protein-based growth, and weight gain out of proportion to linear growth results in poor neurodevelopmental outcomes. Length board for linear measurements is the gold-standard.
Objective: We aim to improve the precision of length measurements by increasing the percentage of measurements with a length discrepancy ≤1cm between nurse and audit measurement. Secondarily, we aim to improve performance of weekly length measurements and maintain length board inventory.
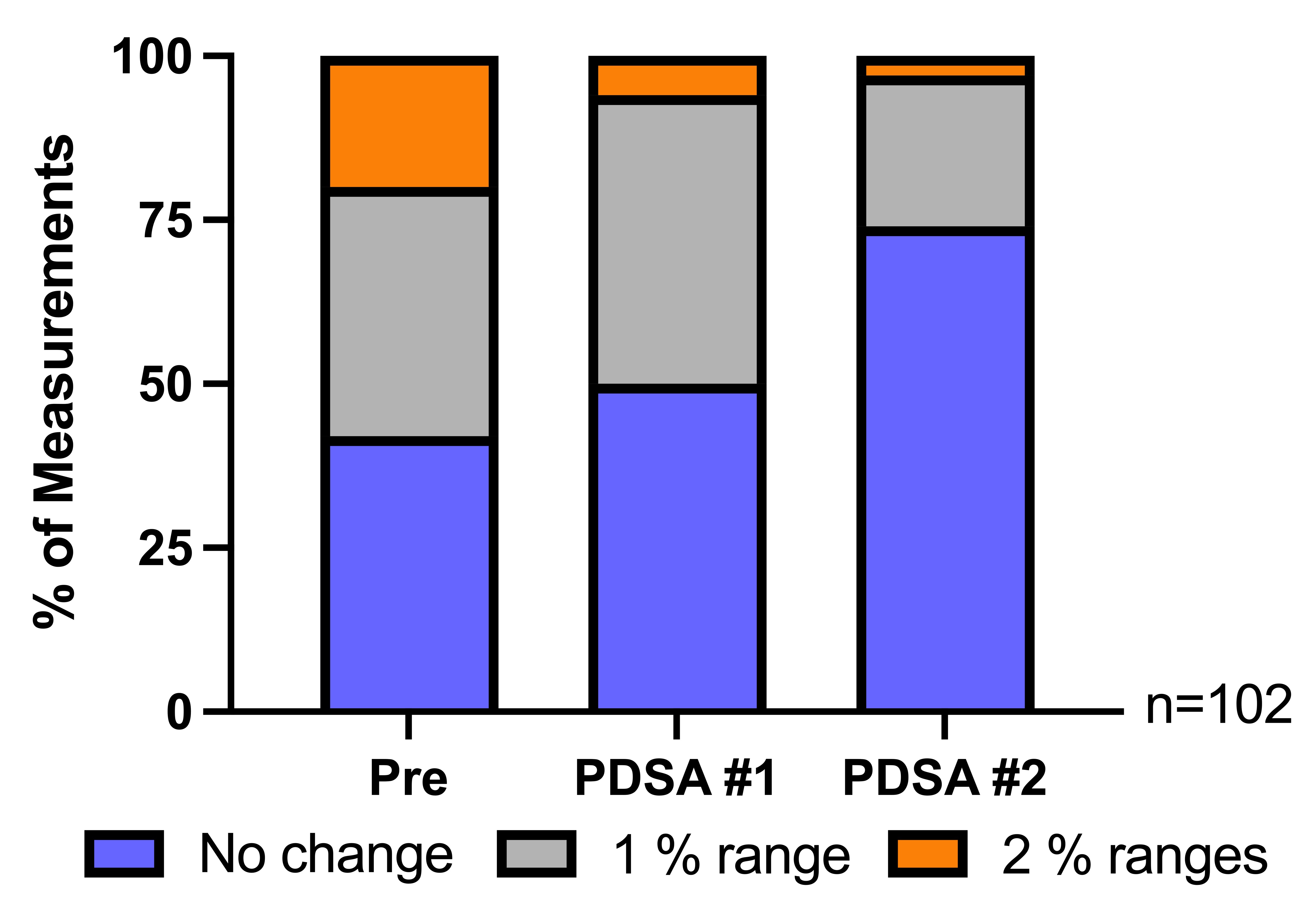
Design/Methods: A quality improvement before and after intervention comparison design was used. Length was measured by the nurse, and blinded audits were performed < 48 hours after using the length board method pre-intervention, post-PDSA#1, and post-PDSA#2. Discrepancies between nurse and audit measurements were recorded. PDSA#1 focused on maintaining inventory while PDSA#2 focused on reinforcing education. Pre- and post-intervention anonymous surveys were administered to NICU nurses. The acceptable level of agreement was set at ≤1cm. Bland-Altman analysis was used to determine limits of agreement and data bias. Chi-square testing was used to determine significance between discrepancies at each time point.
Results: 34 infants were measured at each time point for a total of 102 measurements. There were significant differences in measurements ≤1 cm between the pre-intervention and post-PDSA#2 groups (12 to 25 infants, p=0.003) and between the post-PDSA#1 and post-PDSA#2 groups (11 to 25 infants, p=0.0016). Bland-Altman analysis showed narrower limits of agreement at the conclusion of the study (95% CI 1.33 cm to -2.3 cm). There was a 32% improvement in infants that had consistent length percentiles between nurse and audit measures (42%, 74%, p=0.012) and an increase in performance of weekly length measurements at the conclusion of the PDSA cycles (80%, 90%, p=0.6881).
Conclusion(s): In clinical practice, measurement of neonatal length is often imprecise, leading to erroneous assessment of clinical status. Our interventions more than doubled the precision of linear measurements and maintained board inventory. Increases in the number of weekly length measurements were noted throughout the study, however, further investigation is needed to determine correlation with interventions. Long-term evaluation of our interventions can determine the sustainability of methods. Future PDSA cycles will focus to alleviate resource stress and improve ease-of-use of the length boards.
.jpg)