Emergency Medicine
Session: Emergency Medicine 8: Mental Health
586 - CAUTION: National Patient Safety Goals suggest selective suicide screening for youth with known mental/behavioral health concerns…but is that enough?
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 586
Publication Number: 586.2154
Publication Number: 586.2154

Steven C. Rogers, MD, MS
Pediatric Emergency Medicine Physician
Connecticut Children's Medical Center
Glastonbury, Connecticut, United States
Presenting Author(s)
Background: Suicide is a leading cause of death for ages 10-18. The Joint Commission requires suicide risk screening in healthcare settings such as Pediatric Emergency Departments (PEDs). We developed a UNIVERSAL screening program in our PED. We know that positive suicide risk screens and mental/behavioral health (MBH) patient type puts patients at greater risk for returning to the PED with subsequent suicidal thoughts/behaviors. These conclusions have been drawn from selective screening methods and do not consider the interplay between screening risk and patient type (medical vs MBH).
Objective: We sought to identify those at greatest risk of returning to a PED within 90 days, considering suicide screening risk level and patient type provided at the sentinel visit.
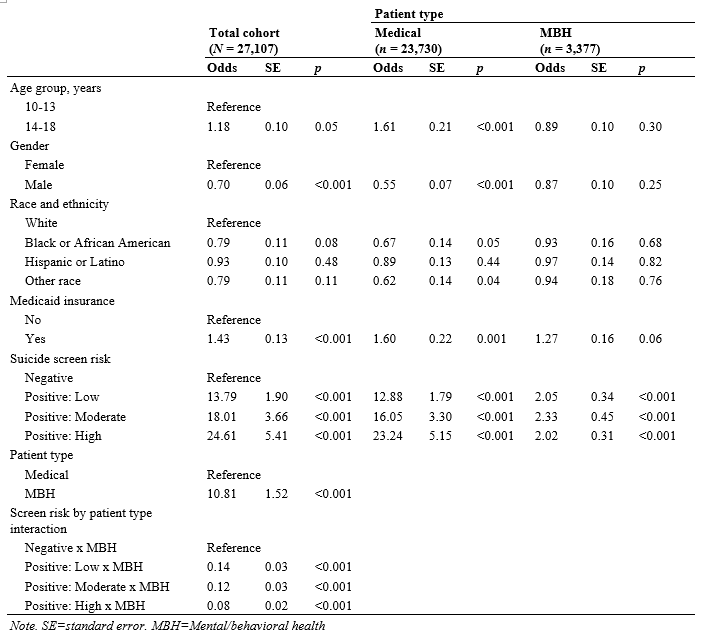
Design/Methods: We examined records for patients 10-18 years who were screened for suicide risk in an urban PED between September 2019-July 2023. We created a logistic regression predicting return rates to the PED with suicidal thoughts/behaviors within 90 days based upon screening risk level, medical vs MBH type, and their interaction, controlling for demographic characteristics.
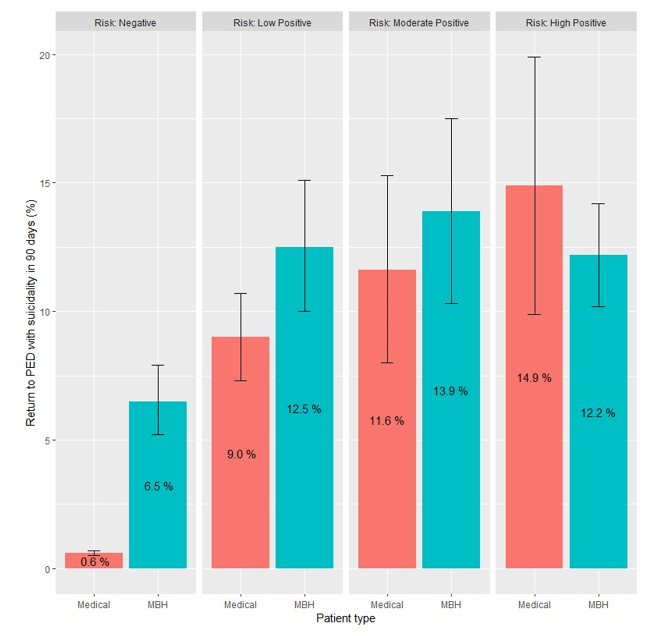
Results: Of 27,107 patients, 13.3% (n=3,603) screened positive for suicide risk. There were significant interactions between screening risk and chief complaint (ps < 0.001). Among medical patients, those with positive screens were 13 times (low risk), 18 times (moderate risk) and 23 times (high risk) more likely to return to the PED within 90 days compared to those with negative screens. Among MBH patients, those with a positive screen were 2.0 times more likely to return compared to negative screens (ps < 0.001) (Table 1). Rates of return did not differ significantly by patient type for positive screen results (10.3%-12.9%;ps>0.09); while rates for MBH patients were significantly higher (6.5%) compared to medical patients (0.6%, p<.001) and negative screens (Figure 1).
Conclusion(s): We concluded that ALL patients with positive suicide screens in a PED, are at increased risk of returning to the PED for subsequent suicidal thoughts/behaviors within 90 days. Medical patients with positive suicide screens return to the PED at predictable rates based on risk level and these rates were concerning and similar to MBH patients. We suggest that screening for suicide amongst youth should be universal. Future studies should also determine and alleviate the barriers that patients, including medical patients, may be experiencing in addressing suicide risk after leaving a PED and which may be leading to return visits.