Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 6
54 - Improving Compliance of Transfer Reconciliation Completion
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 54
Publication Number: 54.2902
Publication Number: 54.2902

Karen Dermer, DO (she/her/hers)
Chief Resident
Renaissance School of Medicine at Stony Brook University
Port Jefferson Station, New York, United States
Presenting Author(s)
Background: Medication errors are a common source of error in the health care field. The most vulnerable time for these errors to occur is during transition of care.1 Transitions occur within the hospital between units or between inpatient to outpatient settings. One study reviewing medication reconciliations during internal hospital transfers indicated that as many as 62% of patients had at least one error, with 36.4% of those errors having the potential to cause harm to the patient.2
Objective: Our objective was to increase the frequency of completed transfer reconciliations (TRs) from the Pediatric Intensive Care Unit (PICU) to the acute pediatric, adolescent, or pediatric hematology/oncology unit by at least 30% between July 2021 and May 2023. Reconciliations are done by residents at the time of unit transfer and include reconciling medications as well as other nursing orders.
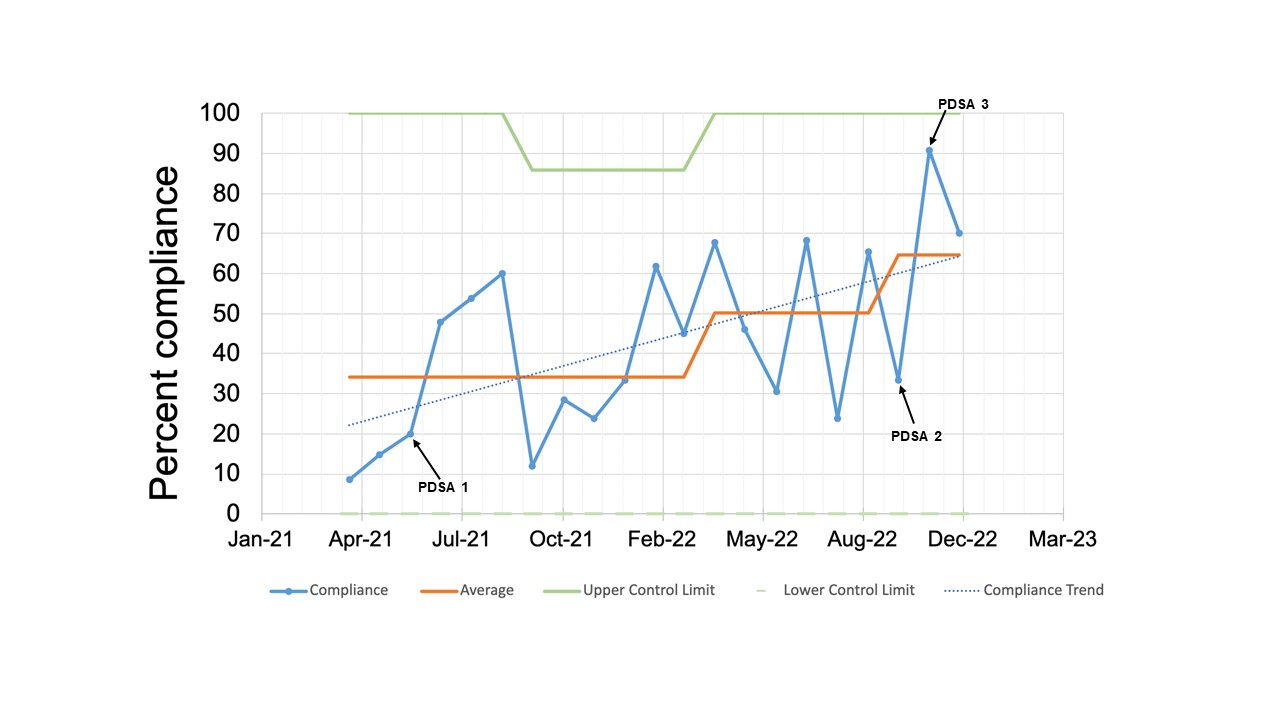
Design/Methods: Utilizing several Plan-Do-Study-Act (PDSA) cycles incorporating both in-person and electronic education, as well as visual and electronic reminders, we were able to improve the percentage of TRs completed. Furthermore, this increase showed a good degree of sustainability despite some ongoing variability in the process.
Results: Results from the first PDSA cycle showed an increase in the percentage of TRs completed from 20% to 47.8%. Data following PDSA cycle 2 and 3 showed an increase in compliance between 70-90%. While there was variation in the percentage, the average compliance remained well above our projected goal of increasing compliance by 30%.
Conclusion(s): Though education and demonstration are not the strongest tools to affect permanent change, we demonstrated their ability to alter workflows to improve compliance with the TR process. Our current PDSA continues to focus on visual aids around workstations to function as additional reminders to complete the TR process. To promote long term sustainability, we continue to investigate the possibility of future changes that will include more human factor integration with forcing functions in the EMR. Further research will be needed to show whether this intervention prevents medication errors or decreases costs.